Understanding Angina: When Your Heart Sends Warning Signals
Just this morning, Mr. Rahman sat across from me, pressing his fist against his chest. “Doctor, it feels like an elephant sitting right here,” he said, his eyes wide with concern. He’d been experiencing this crushing sensation for three weeks, always when walking up the hill to his mosque. The fear in his voice was something I hear almost daily – that unmistakable worry that something’s seriously wrong with the heart. And you know what? He was right to come in. What Mr. Rahman was experiencing was classic angina, and catching it early probably saved his life.
I’ve been treating patients with angina for over 15 years now, and if you’re reading this late at night, worried about that strange chest discomfort you’ve been having, I want you to know you’re not alone. Every week, I see at least a dozen patients with similar concerns. Some turn out to have angina, others don’t, but all of them deserve clear, honest answers about what’s happening in their bodies.

What Angina Really Is – Let Me Break This Down
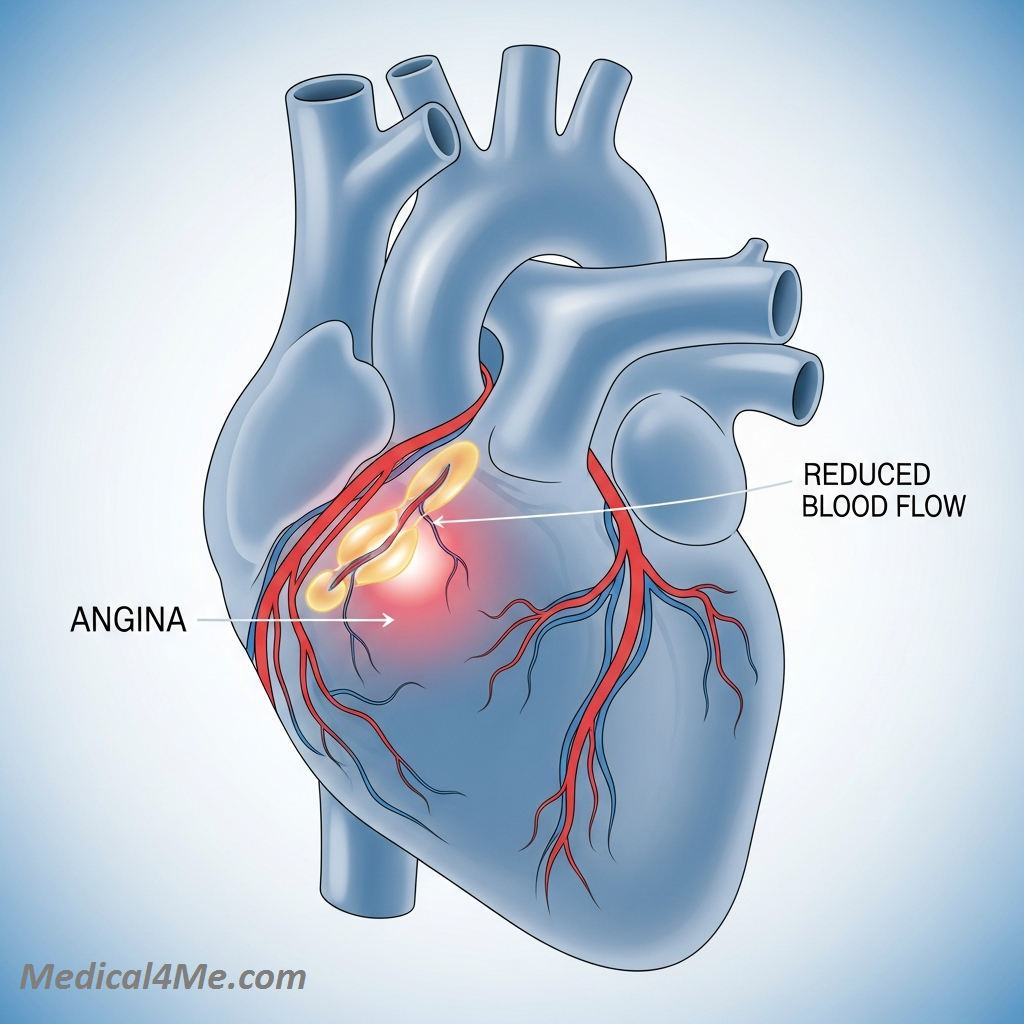
You’ve probably read that angina is chest pain caused by reduced blood flow to the heart. But what does that actually mean?
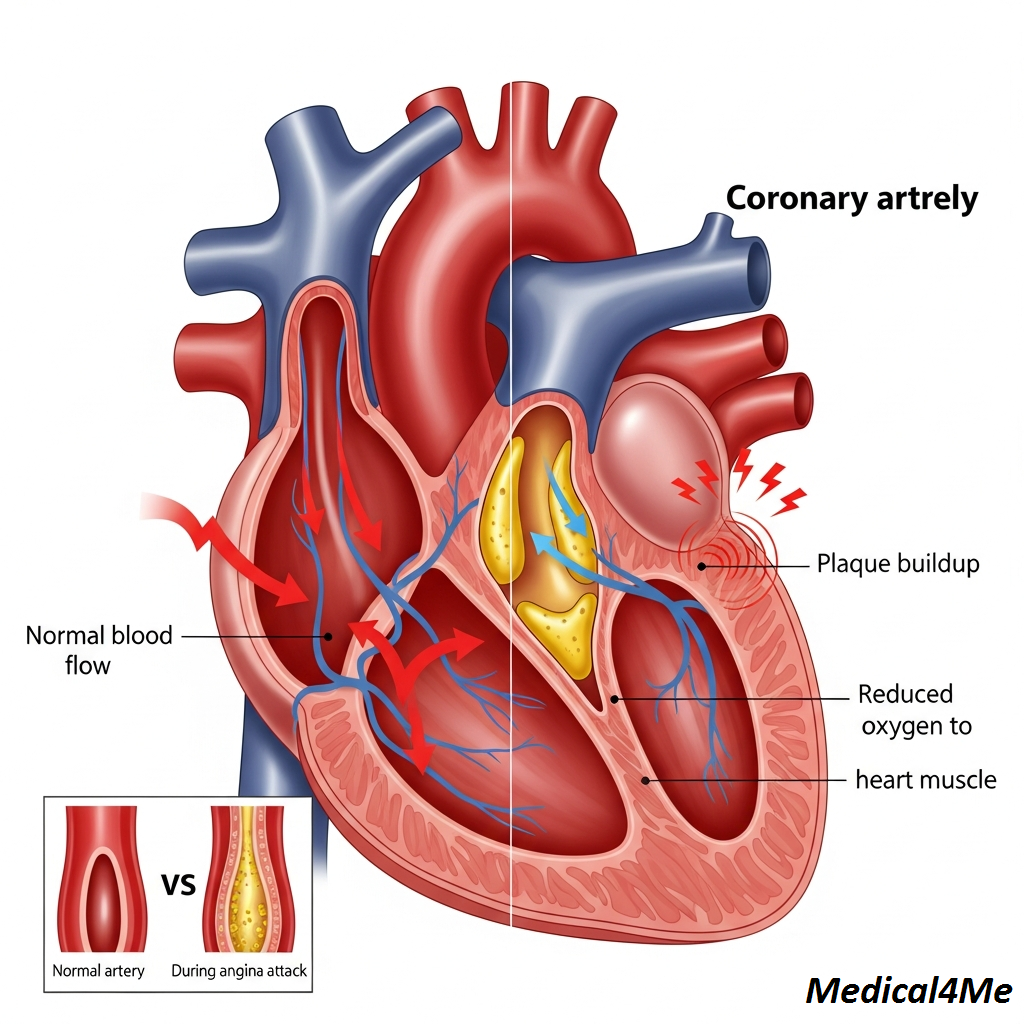
Actually, let me explain this better – imagine your heart as a busy city that never sleeps. The coronary arteries are like the main highways bringing in supplies (oxygen and nutrients) to keep everything running. Now, when these highways get narrowed by traffic jams (plaque buildup) or construction work (artery spasms), parts of the city don’t get their deliveries on time. The city doesn’t shut down completely – it just sends out distress signals. That distress signal? That’s angina.
It’s not a heart attack, though many of my patients initially think it is. With angina, the “city” is struggling but still functioning. The roads are narrowed but not completely blocked. Once the traffic clears – usually when you rest and your heart doesn’t need as much oxygen – the distress signal stops. A heart attack, on the other hand, is when the highway gets completely blocked and part of the city starts dying from lack of supplies.
The tricky thing about angina is that it’s both a condition and a warning. Think of it like your car’s check engine light – it’s telling you something needs attention before it becomes a bigger problem. Some patients have stable angina for years and manage it perfectly well with medication and lifestyle changes. Others might have unstable angina that needs immediate intervention.
What really gets to me is when I see younger patients – people in their 40s or even late 30s – coming in with angina symptoms. We’re seeing it more often now, especially in people with diabetes or those who’ve been under chronic stress. The good news? We have more treatment options than ever before.
How Angina Actually Feels – Beyond the Textbook Symptoms
Mrs. Patel came in last week describing what she thought was severe indigestion. “It’s this heavy, burning feeling,” she said, “like I’ve eaten too much, but it happens when I’m walking, not after meals.” This is exactly why angina can be so confusing – it doesn’t always feel like what you’d expect.
The classic description is chest pressure or squeezing, but honestly? Only about half my patients describe it that way.
Some say it feels like:
- A tight band around their chest
- Someone standing on their ribcage
- A hot, burning sensation (often mistaken for heartburn)
- A dull ache that’s hard to pinpoint
- Breathlessness without any chest sensation at all
Women especially tend to have what we call “atypical” symptoms, though I hate that term – if half the population experiences something, how is it atypical? They might feel unusually tired, nauseated, or have pain in their jaw, neck, or back instead of their chest. I had a patient, Mrs. Chen, who only felt pain in her left shoulder blade. She’d been seeing a physiotherapist for months before someone thought to check her heart.
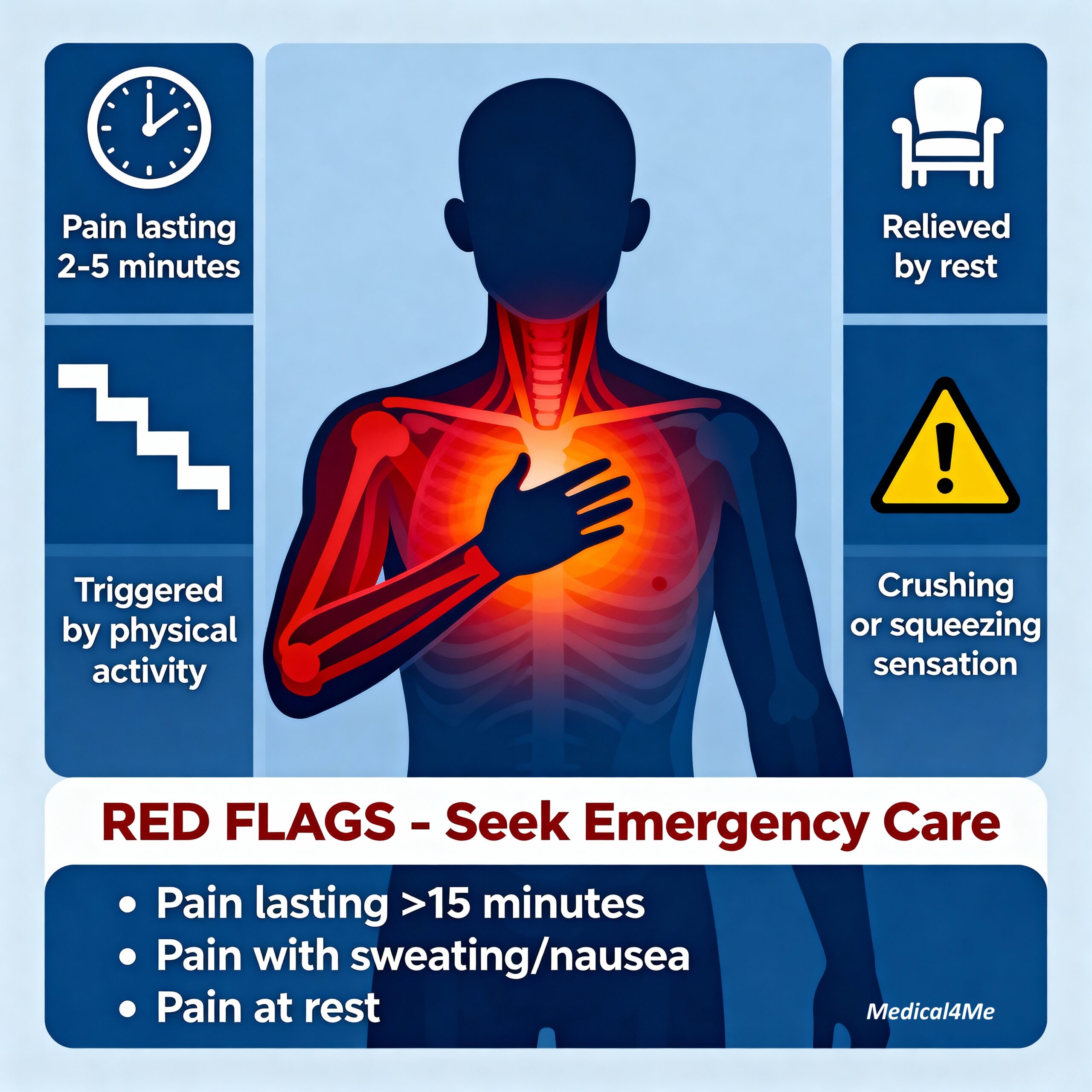
The timing is often more telling than the sensation itself. Does it happen when you’re physically active and stop when you rest? That’s a classic angina pattern. Does it last for a few minutes (usually 2-5) rather than hours? Again, typical angina. If you’re lying in bed and suddenly get chest pain that lasts for hours, that’s probably not angina – though you should still get it checked.
One thing that surprises patients is how predictable stable angina can be. Mr. Thompson told me last month, “I know exactly when it’ll happen – at the 10-minute mark of my morning walk, like clockwork.” That predictability is actually reassuring from a medical standpoint. It’s the unpredictable, rest-occurring, or progressively worsening symptoms that worry me more.
Why Angina Happens – The Real Culprits
So why do some people get angina while others with similar lifestyles don’t?
The main villain here is usually atherosclerosis – the gradual buildup of fatty deposits in your coronary arteries. But it’s not just about eating too much fast food, despite what some websites claim. Atherosclerosis is a complex process involving inflammation, genetics, and yes, lifestyle factors.
Here’s what typically contributes:
- High blood pressure (the silent artery damager)
- High cholesterol (especially the bad LDL type)
- Diabetes (high blood sugar damages artery walls)
- Smoking (I can’t stress this enough – it’s like sandpaper on your arteries)
- Family history (if your parents had heart disease, you’re at higher risk)
But here’s where it gets interesting – we still don’t fully understand why some people with squeaky-clean arteries still get angina. There’s something called microvascular angina where the tiny blood vessels in the heart don’t work properly, even though the main highways look fine on an angiogram. We also see coronary artery spasm, where the arteries suddenly tighten for reasons we’re still figuring out. Stress seems to play a role, but the exact mechanism remains a bit of a medical mystery.
Age plays its part too. Men typically start showing up in my office with angina symptoms after 45, women after 55. But I’m seeing exceptions more frequently now. Just last month, a 38-year-old software developer came in with classic angina symptoms. His job stress, combined with a family history and pre-diabetes, had accelerated everything.
The Diagnostic Journey – What Actually Happens
When someone comes to me with suspected angina, we don’t just jump to complex tests.
First, we talk. Really talk. I want to know everything – when the pain happens, what it feels like, what makes it better or worse. This conversation often tells me more than any test. Then comes the physical exam, though honestly, if you’re sitting comfortably in my office, it’ll probably be normal. Angina is sneaky like that.
The ECG (electrocardiogram) comes next – those sticky patches on your chest that record your heart’s electrical activity. If you’re not having symptoms right then, it might be completely normal. Don’t worry, that doesn’t mean we don’t believe you. We usually move on to a stress test, where we either have you walk on a treadmill or give you medication that makes your heart work harder while we monitor everything.
Mr. Kumar had his stress test last week and asked me, “Why can’t you just look inside my arteries straight away?” Good question. We could do an angiogram (threading a tiny camera through your arteries), but it’s invasive and has small risks. We prefer to start with non-invasive tests first. Though nowadays, we have CT coronary angiography – a special scan that can show your arteries without going inside them. It’s brilliant for the right patients.
Blood tests help too. We check your cholesterol, blood sugar, and markers of heart damage. Sometimes we do an echocardiogram – an ultrasound of your heart – to see how well it’s pumping. The whole diagnostic process usually takes a few weeks from start to finish, depending on waiting lists and how urgent your symptoms are.
What bothers me is when websites claim you need every test under the sun immediately. That’s not how good medicine works. We tailor the investigation to your specific situation.
Treatment Options – The Real Deal on What Works
Let’s talk about treatment, including something many doctors don’t mention – the costs involved.

Medications That Actually Help
First line is usually a combination of drugs. Nitrates (like the famous nitroglycerin tablets) work instantly by opening up your blood vessels. I give most patients a spray or tablets to carry – about $20-30 per month without insurance. You pop one under your tongue when angina strikes, and within minutes, you’re better. Beta-blockers, which slow your heart rate and reduce its oxygen demand, cost around $10-40 monthly.Beta-blockers work particularly well for exercise-induced angina.
Calcium channel blockers are another option, especially if you can’t tolerate beta-blockers. They relax your arteries and reduce the heart’s workload. Generic versions run about $15-50 monthly. We almost always add aspirin (dirt cheap at $5 monthly) to prevent blood clots, and statins to lower cholesterol – even if your levels seem okay. Statins do more than just lower cholesterol; they stabilize the plaques in your arteries.
Procedures When Medications Aren’t Enough
Sometimes medications aren’t enough. That’s when we consider procedures.
Angioplasty (opening blocked arteries with a balloon and usually placing a stent) can cost $30,000-50,000 in the US without insurance, though it’s often covered. Recovery is quick – most patients go home the next day. Bypass surgery is the bigger gun – we create new routes around blocked arteries using vessels from elsewhere in your body. It’s major surgery, costing $70,000-150,000, with a longer recovery of 6-12 weeks. But for the right patients, it’s life-changing.
Lifestyle Changes That Don’t Cost a Fortune
Here’s what I tell every patient: the most powerful treatment might be the cheapest. Walking 30 minutes daily costs nothing and can reduce angina episodes by half. The Mediterranean diet – lots of vegetables, fruits, whole grains, and olive oil – isn’t fancy or expensive. World Health Organization guidelines emphasize these lifestyle modifications as first-line treatment.
I had a patient, Mr. Ali, who couldn’t afford all his medications initially. We focused on lifestyle changes – he quit smoking (hardest but most important), started walking, and switched to a healthier diet. His angina improved by 70% before we even optimized his medications. Don’t get me wrong – most people need medications too. But never underestimate the power of lifestyle changes.
Red Flags – When to Drop Everything and Get Help
Listen, I don’t want to scare you, but there are times when chest pain isn’t something you wait out.
Call an ambulance immediately if:
- Chest pain lasts more than 15 minutes
- Pain doesn’t improve with rest or nitroglycerin
- You’re sweating, nauseated, or feel like you’re going to faint
- The pain is the worst you’ve ever felt
- It’s different from your usual angina pattern
Last week, Mrs. Roberts called me saying her angina felt “different” – sharper and not going away with her usual spray. I told her to call 911 immediately. Good thing too – she was having a heart attack. Her instinct that something was different saved her life. Trust your gut. If something feels wrong, it probably is.
What frustrates me is when patients wait hours or even days with worsening symptoms because they don’t want to “bother” anyone. You’re not bothering us – this is literally what we’re here for. CDC statistics show that getting treatment within the first hour of a heart attack can save your life and preserve heart function.
Common Questions I Get Every Week
“Can I still have sex if I have angina?”
Usually, yes. If you can climb two flights of stairs without symptoms, you’re generally okay for sexual activity. Some patients keep their nitroglycerin spray nearby just in case. Just don’t use Viagra-type drugs if you’re on nitrates – that combination can dangerously drop your blood pressure.
“Will I have this forever?”
Not necessarily. Some of my patients have reversed their angina through aggressive lifestyle changes and medication. Others manage it so well they forget they have it. Mr. Jackson told me yesterday he hasn’t had symptoms in two years since his stent and medication adjustment.
“Can stress cause angina even if my arteries are clear?”
Absolutely. Emotional stress can trigger coronary artery spasm or affect those tiny blood vessels I mentioned earlier. I’ve seen it many times, especially in younger women. Mayo Clinic research confirms that stress management can significantly reduce angina episodes in some patients.
“Is angina hereditary?”
The tendency to develop coronary artery disease can run in families, yes. But having a parent with angina doesn’t mean you’re doomed. You can modify your risk through lifestyle choices. I always tell patients with family history to be extra vigilant about prevention.
Your Next Steps – Let’s Get Practical
If you’ve made it this far, you’re probably wondering what to do next.
First, see your doctor. I know that sounds obvious, but you’d be surprised how many people suffer in silence. Bring a symptom diary – write down when you get chest discomfort, what you were doing, how long it lasted, and what helped. This information is gold for diagnosis.
Be honest about your symptoms. Don’t downplay them or try to be brave. We need the full picture to help you properly. Ask about cardiac rehabilitation programs if you’re diagnosed with angina – they’re incredibly helpful and often covered by insurance.
Start making changes today, even small ones. Take a 10-minute walk. Skip that cigarette. Choose grilled chicken over fried. These little changes add up. And please, don’t rely on Dr. Google for treatment advice – every case of angina is different, and what works for one person might not work for you.
The key takeaway? Angina is your heart’s warning system, not a death sentence. With proper treatment and lifestyle changes, most people with angina live long, active lives. If you’re experiencing chest discomfort with exertion that goes away with rest, please see your doctor.

💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.