Stroke Signs and Treatment: A Doctor’s Guide to Survival
Every 40 seconds, someone in the United States has a stroke. Every 3 minutes and 14 seconds, someone dies of one. In my clinical experience working in emergency rooms, those seconds between the onset of symptoms and the moment treatment begins are what we call “brain time.” The clock isn’t just ticking; it’s roaring.
But here is the good news: a stroke is no longer a guaranteed life sentence of disability. With rapid advances in stroke signs and treatment protocols, we are seeing patients walk out of hospitals who, just a decade ago, might not have survived. Understanding the early warning signs and knowing exactly what to do can literally mean the difference between a full recovery and permanent damage.
If you or a loved one is navigating this frightening diagnosis, take a deep breath. You aren’t alone in this journey. This guide is designed to walk you through everything—from that terrifying first moment to the hopeful road of recovery—stripping away the complex medical jargon and giving you the clear facts you need right now.
What Exactly Is a Stroke?
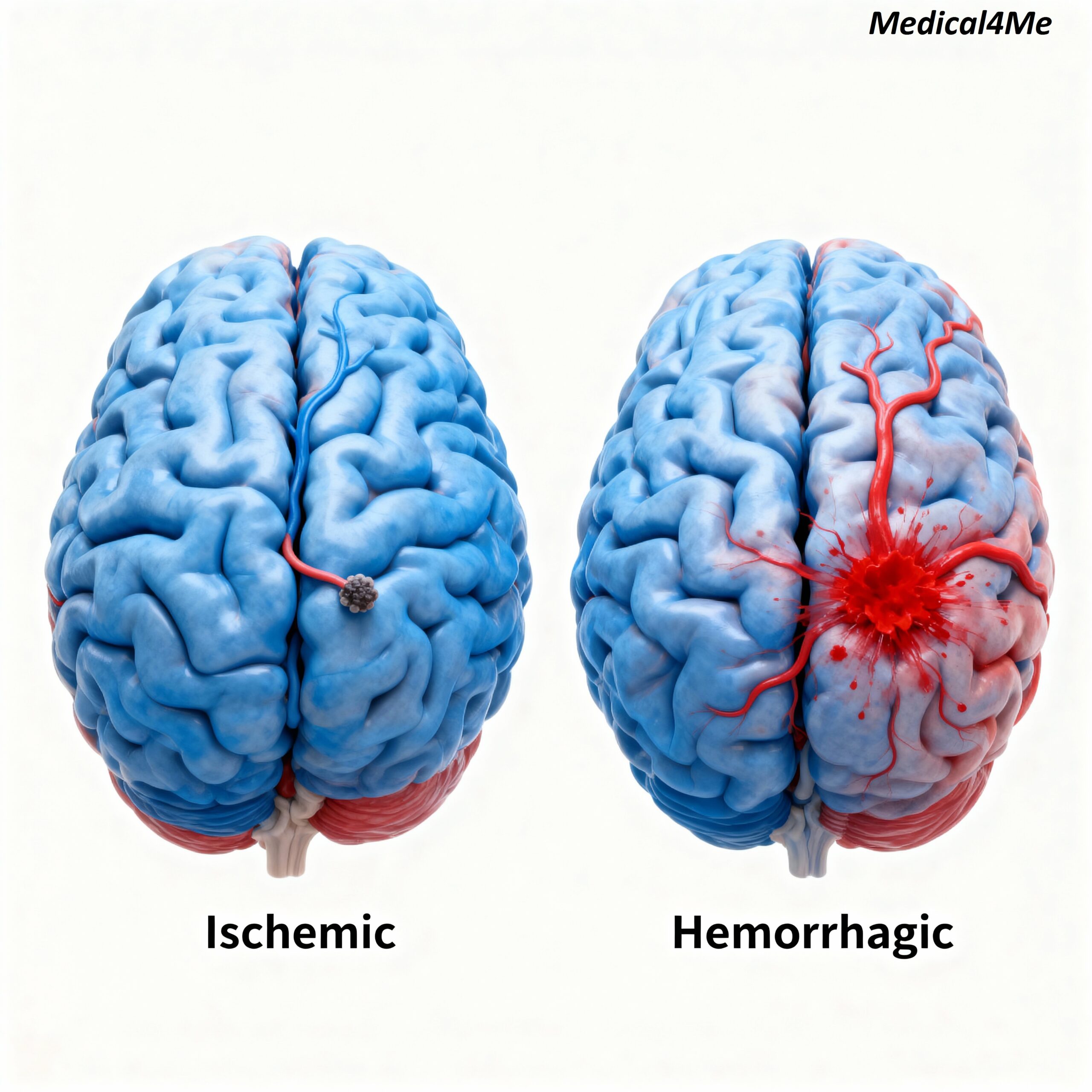
Think of your brain as a bustling city. The blood vessels are the highways delivering essential fuel (oxygen and nutrients) to the buildings (brain cells). A stroke happens when one of those highways gets blocked or bursts.
There are two main types you need to know about:
- Ischemic Stroke: This is the most common type, accounting for about 87% of cases. It happens when a clot blocks blood flow to the brain—like a traffic jam on the highway.
- Hemorrhagic Stroke: This occurs when a blood vessel ruptures and bleeds into the brain. It’s less common but often more severe.
There is also something called a Transient Ischemic Attack (TIA), often called a “mini-stroke.” But honestly, I dislike that term because it makes it sound minor. A TIA is a major warning sign that a full stroke is coming.
Why This Matters
A stroke doesn’t just happen to a person, it happens to a family. It happens to the wife who suddenly has to become a nurse. It happens to the son who has to lift his father out of a wheelchair. The “Brain Attack” steals memories, movement, and dignity. But here is the thing: It is treatable. But only if you are fast.
Recognizing Symptoms and Signs: The FAST Protocol
When it comes to stroke signs and treatment, speed is your best friend. I cannot stress this enough: time lost is brain lost. In the medical community, we rely on the FAST acronym, and you should too. It’s simple, effective, and it saves lives every single day.
- F – Face Drooping: Ask the person to smile. Does one side of the face droop or feel numb?
- A – Arm Weakness: Ask them to raise both arms. Does one arm drift downward?
- S – Speech Difficulty: Is their speech slurred? Can they repeat a simple sentence like “The sky is blue” correctly?
- T – Time to Call 911: If the person shows any of these signs, even if the symptoms go away, call 911 immediately. Do not drive to the hospital. An ambulance can start treatment on the way.
But wait, there’s more. While FAST covers the basics, other signs can be subtler depending on which part of the brain is affected.
The Traffic Light of Symptoms
Here is a way to visualize severity based on what I’ve seen in patients:
- 🟢 Mild/Vague (Proceed with Caution): Sudden dizziness, loss of balance, or a sudden severe headache with no known cause. These are easily dismissed as dehydration or fatigue. Don’t ignore them.
- 🟡 Moderate (Warning): Sudden confusion, trouble understanding speech, or trouble seeing in one or both eyes. This is often a sign of a TIA or developing stroke.
- 🔴 Severe (Emergency): Complete paralysis on one side of the body, loss of consciousness, or the “worst headache of your life.” This is a code red.
⚠️ When to Seek Medical Help
Here is the thing: You are not a doctor, and you shouldn’t try to diagnose this at home. If you suspect a stroke, call 911 immediately. Do not take an aspirin. Do not wait to see if it gets better. Every minute left untreated destroys approximately 1.9 million brain cells.
According to CDC, acting fast can minimize long-term disability.
Understanding Causes and Risk Factors
So, why does this happen? Well, it’s usually not just one thing. It’s often a combination of lifestyle factors and genetics building up over time. I’ve treated patients who ran marathons and patients who never exercised—strokes can affect anyone, but certain factors definitely stack the deck against you.
The leading cause, hands down, is high blood pressure. It puts constant stress on your artery walls, making them prone to damage or bursting. But let’s look at the broader picture:
- High Cholesterol: Plaque builds up in arteries, narrowing the path for blood.
- Smoking: It thickens your blood and increases plaque buildup.
- Diabetes: High blood sugar damages blood vessels over time.
- Obesity and Inactivity: These contribute to all the factors above.
- Atrial Fibrillation (AFib): This irregular heartbeat can cause clots to form in the heart and travel to the brain.
I often tell my patients that managing these risks is like investing in a 401(k) for your health. You might not see the payout immediately, but 20 years from now, you’ll be incredibly glad you did.
The Diagnostic Journey
When a patient arrives at the ER with potential stroke symptoms, the atmosphere shifts. It becomes a choreographed dance of precision. The doctor needs to answer two questions immediately: Is it a stroke? And if so, which kind?

The first step is almost always a CT Scan. This imaging test is fast and can quickly rule out a hemorrhagic stroke (bleeding). Why does this matter? Because the medication used to dissolve clots (tPA) would be fatal if given to a patient who is bleeding.
Following that, an MRI might be ordered for a more detailed view of the brain tissue. Doctors may also perform a Carotid Ultrasound to check for narrowing in the neck arteries or an Echocardiogram to see if clots are coming from the heart.
Treatment Options Comparison
Treatment depends entirely on the type of stroke and how much time has passed. This is where modern medicine truly shines. We have tools now that didn’t exist a generation ago.
For ischemic strokes, the gold standard is tPA (tissue plasminogen activator). It’s an IV medication that dissolves the clot and restores blood flow. But there’s a catch: it must typically be administered within 3 to 4.5 hours of symptom onset. This is why knowing the time symptoms started is crucial.
For larger clots, doctors might perform a mechanical thrombectomy. This involves threading a catheter through an artery in the groin up to the brain to physically grab and remove the clot.
| Treatment Option | Best For | Time Window | Effectiveness |
|---|---|---|---|
| tPA (IV Medication) | Small to medium clots (Ischemic) | 3 – 4.5 hours | High if given early |
| Mechanical Thrombectomy | Large vessel occlusions | Up to 24 hours (in some cases) | Very High for large clots |
| Surgical Clipping/Coiling | Aneurysms (Hemorrhagic) | Varies (Emergency) | Life-saving for bleeds |
| Blood Pressure Management | All Stroke Types | Immediate & Long-term | Preventative & Stabilizing |

Recovery doesn’t end when the ambulance leaves. Post-stroke care involves aggressive management of risk factors to prevent a second event. See more on Medical4Me to understand how heart health connects to brain health.
Prevention Strategies
Here is the empowering part: up to 80% of strokes are preventable. That is a staggering number. It means you have more control than you think.
Simple Lifestyle Shifts
You don’t have to run a marathon tomorrow. Start small. Lower your sodium intake to keep blood pressure in check. Aim for 30 minutes of walking five days a week. If you smoke, I know it’s hard to quit, but it is the single best thing you can do for your arteries.
Also, keep an eye on your numbers. Know your blood pressure, your cholesterol, and your blood sugar. These are the silent indicators of what’s happening inside your vessels.
Patient Story: Robert’s Second Chance
I remember meeting Robert, a 54-year-old accountant, in the ICU. He was lucky. His wife noticed his speech was slurred during breakfast—he kept saying “coffee” but it sounded like “cah-fee”—and called 911 immediately. He arrived at the hospital within 45 minutes.
Because he arrived so quickly, we were able to administer tPA. The clot dissolved. Three days later, Robert walked out of the hospital with only a mild weakness in his left hand. “I thought I was just tired,” he told me later. “If my wife hadn’t made that call, I wouldn’t be holding my grandson today.” Robert’s story is a testament to the power of awareness.
Latest Research & Developments
The field of neurology is moving fast. Recent studies from 2023 and 2024 are exploring neuroprotective drugs—medicines that can shield brain cells from death even while blood flow is blocked. There is also fascinating research into using AI to detect strokes on CT scans faster than the human eye, shaving precious minutes off diagnosis times.
Furthermore, stem cell therapy is being investigated for chronic stroke patients, offering hope for regenerating damaged brain tissue months or even years after the event. NIH
Frequently Asked Questions
Conclusion
Navigating the world of stroke signs and treatment can feel overwhelming, but knowledge is your armor. Remember the FAST protocol. Listen to your body. And if you are currently on the road to recovery, be patient with yourself. The brain is incredibly resilient, and with the right support, rehabilitation, and determination, life after a stroke can be full and meaningful.
Don’t wait for a crisis to prioritize your vascular health. Schedule that check-up, take that walk, and share this information with your family. You might just save a life. For more diseases Explore Diseases.
Medical Disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on Medical4Me.com.

💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.