Bronchitis
Hey there, my friend. I know it’s late, and I can hear the worry in your voice, even over text. That cough sounds absolutely relentless, and I’m glad you reached out. Let’s talk about it. Forget the sterile medical jargon for a minute. Let’s just have a real conversation about what’s likely going on, what it means, and how you can start feeling better.
You mentioned you think you have bronchitis, and that’s a word that can sound pretty intimidating. But I want to empower you with good, clear information so you can take control of the situation. Tonight, you’re not just a patient; you’re my friend, and I’m here to walk you through this, step-by-step. So, grab a warm cup of tea, get comfortable, and let’s unravel this together.

What Bronchitis Really Is (And My Highway Analogy)
Alright, first things first. Let’s demystify the term bronchitis.
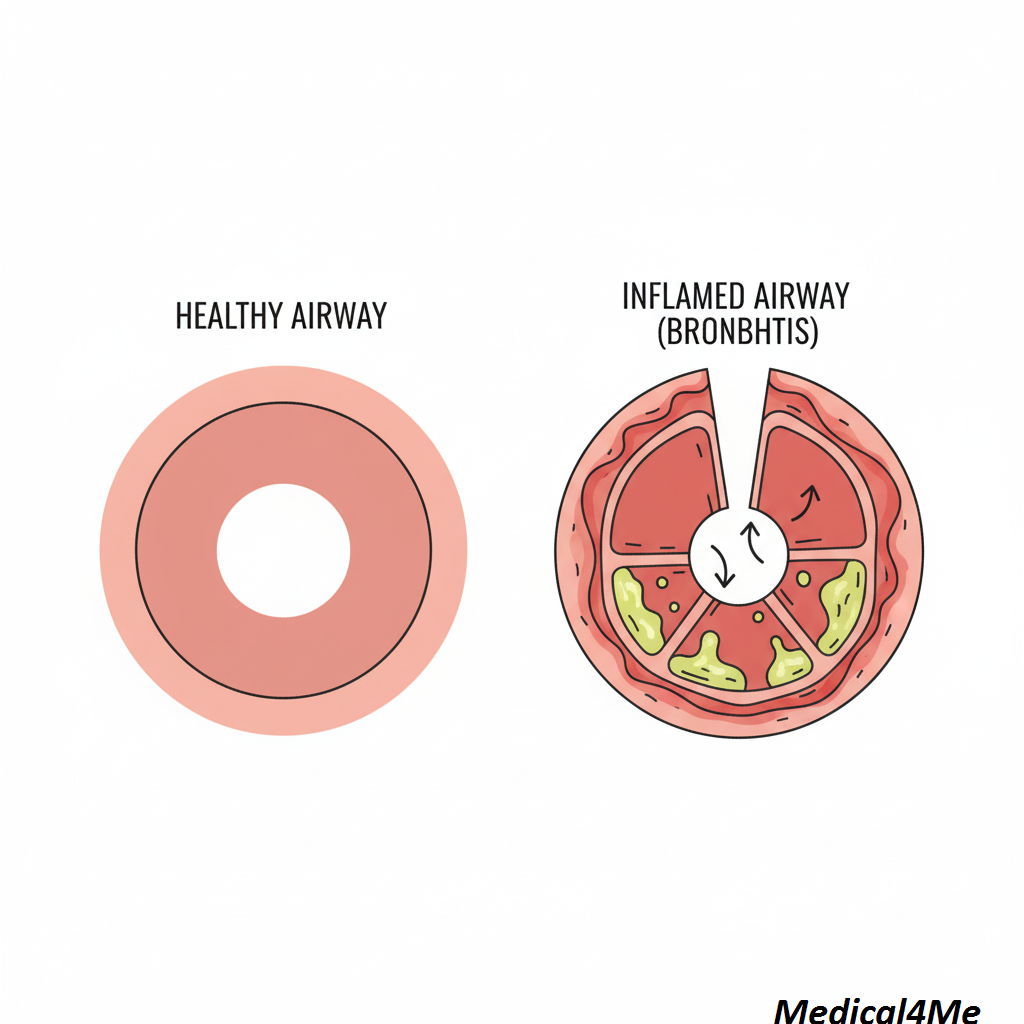
Think of your lungs as a massive, upside-down tree. The trunk is your windpipe (the trachea), and it splits into large branches called bronchial tubes. These branches get smaller and smaller, delivering air to the tiny leaf-like air sacs (alveoli) where the magic of oxygen exchange happens.
Now, imagine those bronchial tubes aren’t branches, but a city’s intricate highway system. Day in and day out, traffic—in this case, the air you breathe—flows smoothly in both directions. It’s a perfect, efficient system.
Bronchitis is what happens when there’s a major traffic jam on those highways. The lining of your bronchial tubes gets inflamed and swollen. It’s like a massive, messy spill on the freeway. Because of this irritation, your body produces a ton of extra mucus to try and protect the area and wash away the irritant. This combination of swelling and thick mucus narrows your airways, causing a major gridlock. The air can’t get through easily. And what’s your body’s natural response to a roadblock? It tries to clear it forcefully. That’s your cough. That deep, chesty, relentless cough is your body’s tow truck, desperately trying to clear the mucus and debris off the highway so traffic can flow again.
Most of the time, we’re talking about acute bronchitis. This is the short-term kind, usually sparked by the same viruses that cause colds and the flu. It’s incredibly common and typically resolves on its own. Then there’s chronic bronchitis, which is a more serious, long-term condition, often linked to smoking, and is part of a group of diseases called COPD. For our chat tonight, we’ll focus mostly on the acute kind, because that’s what I suspect you’re wrestling with.
Recognizing the Symptoms: Is This What You’re Feeling?
My first thought when a patient comes in describing a “chest cold” is to mentally run through a checklist. Does this line up with classic acute bronchitis? It’s often a frustrating experience because you feel absolutely drained, but there isn’t a magic pill to fix it instantly.
Let me tell you about a patient of mine, Amina. She’s a 42-year-old graphic designer who came to see me last winter. She’d had a simple head cold for a few days—runny nose, sore throat—and just as she thought she was turning a corner, this deep, hacking cough set in. She said it felt like her chest was “on fire” and she couldn’t get a full breath without triggering another coughing fit. That’s a textbook story.
Here’s a look at the classic symptoms. See how many of these feel familiar to you right now:
- The Persistent Cough: This is the star of the show. It can be dry and hacking at first, but it often progresses to a “productive” cough, meaning you’re coughing up mucus. This mucus can be clear, white, yellow, or even greenish.
- Chest Discomfort: You might feel a sense of soreness, tightness, or burning in your chest, especially after a coughing spell. It’s not usually a sharp, stabbing pain, but more of a deep ache from the inflammation and the sheer muscular effort of coughing.
- Fatigue: Your body is working overtime to fight this inflammation. This diverts a massive amount of energy, leaving you feeling profoundly tired and run-down. Don’t underestimate this!
- Shortness of Breath: Because your airways are narrowed, you might feel like you can’t quite catch your breath. You might also hear a slight whistling or wheezing sound when you breathe.
- Low-Grade Fever and Chills: It’s common to have a slight fever (under 100.4°F or 38°C) and feel generally unwell, similar to how you feel with a cold or flu.
- Sore Throat and Body Aches: These often tag along from the initial virus that kicked everything off.
If you’re nodding along to this list, you’re in the right place. This is a very typical presentation, and while it’s miserable, it’s also manageable.
The Root Causes: Where Did This Come From?
Understanding the “why” is key to feeling in control. The overwhelming majority of acute bronchitis cases—we’re talking over 90%—are caused by viruses. These are the same culprits responsible for the common cold and the flu, like rhinoviruses, influenza viruses, and coronaviruses (the non-COVID-19 types, usually).
Because of this, antibiotics are almost always useless against acute bronchitis. It’s like sending a plumber to fix an electrical problem; they’re simply the wrong tool for the job. Using them unnecessarily can lead to side effects and contribute to antibiotic resistance, a huge global health issue.
In a much smaller number of cases, bacteria can be the cause, but this is far less common. We also see bronchitis triggered by environmental irritants. Think about Sophia, a 58-year-old bakery owner I’ve treated for years. She developed chronic bronchitis. For her, it wasn’t a virus; it was years of inhaling fine flour dust combined with a long history of smoking. Her airways are in a state of constant, low-grade inflammation. This is a different beast altogether and requires long-term management, as I’ve covered in recent articles on chronic conditions. For you, right now, a virus is the most likely suspect.
The Diagnostic Journey: How We Know It’s Bronchitis
So, how do we confirm it? Often, the diagnosis is a clinical one, meaning the story you tell and the symptoms you describe are so classic that extensive testing isn’t needed.
However, we have to be detectives. My main job is to make sure it’s not something more serious, like pneumonia, which is an infection inside the lung’s air sacs (the “leaves” of the tree) rather than just the airways (the “branches”). Pneumonia is a more serious condition that often does require antibiotics.
This reminds me of David, a 65-year-old retired librarian. He came in after two weeks of a cough that just wouldn’t quit. He was also feeling more breathless than I liked and had a mild fever that kept lingering. For him, I needed to be more thorough.
Here’s the step-by-step process I typically follow:
- The Medical History: This is the most important step. I’ll ask you a dozen questions. When did the cough start? What does it feel like? Are you coughing anything up? What color is it? Do you have a fever? Any chest pain? Are you a smoker? Your answers paint 90% of the picture for me.
- The Physical Exam: Next, I’ll listen to your lungs with my stethoscope. I’m listening for specific sounds. With bronchitis, I might hear some coarse sounds called “rhonchi,” which are low-pitched gurgling sounds that often clear up after you cough. I might also hear “wheezing,” a high-pitched whistle that indicates narrowed airways. What I’m listening for, and hoping not to hear, are “crackles.” These are fine, popping sounds that can be a sign of fluid in the air sacs, pointing more toward pneumonia, as the Mayo Clinic explains.
- Pulse Oximetry: I’ll clip a small, painless device to your fingertip. This measures the oxygen saturation in your blood. A healthy level is typically 95% or higher. If it’s dropping low, that’s a red flag that your lungs aren’t working efficiently, and we need to investigate further.
- Chest X-ray (If Needed): If I hear something concerning on your exam, if your oxygen is low, if your fever is high, or if the cough has lasted for many weeks, I’ll order a chest X-ray. In a case of simple acute bronchitis, the X-ray will usually look clear. If it shows a shadow or an “infiltrate,” that confirms a diagnosis of pneumonia. For David, his exam was a bit borderline, so we got the X-ray to be safe. Thankfully, it was clear, which gave us both peace of mind.
Treatment Reality: How You Can Start Healing
Alright, here’s the most important part: the action plan. The goal here is twofold: support your body so it can fight off the virus, and manage your symptoms so you’re not completely miserable in the process.
Lifestyle & Home Care: Your Foundation for Recovery
This is honestly where the battle is won. Don’t dismiss these steps as “simple”—they are profoundly effective.
- Hydration is Everything: Drink, drink, drink. Water, herbal tea with honey, clear broth. Fluids help thin out that thick mucus, making it easier for your body to cough it up and clear the “highways.” Dehydration makes mucus stickier and harder to clear.
- Embrace Humidity: A humidifier, especially at night, is your best friend. The moist air soothes your irritated airways and helps loosen congestion. If you don’t have one, a steamy shower can work wonders.
- Rest! Seriously: Your body is in a fight. Pushing through and going to work will only prolong your illness. You need to conserve your energy so your immune system can do its job. Allow yourself to rest.
- Avoid Irritants: This is a big one. Stay away from cigarette smoke (both first and secondhand), strong fumes, dust, and pollution. Your airways are raw and sensitive; don’t provoke them further.
- Honey & Lemon: Don’t underestimate this classic remedy. Honey is a natural cough suppressant and has some antimicrobial properties. A teaspoon in warm water or tea can be incredibly soothing for a sore throat and nagging cough.
Medical Options: When Home Care Isn’t Enough
Sometimes, the symptoms are just too severe to manage with home care alone. To be perfectly honest, the medical community is still exploring the precise mechanisms behind why some people have such a prolonged and severe cough after a virus, but we have tools to help.
Here, we’re not “curing” the virus, but we are managing the inflammation and symptoms. This is where a conversation with your doctor becomes important to see if prescription options are right for you.
Here’s a comparison of two common approaches:
| Treatment Approach | Pros | Cons |
|---|---|---|
| Over-the-Counter (OTC) Symptom Relief | Easily accessible; allows you to target specific symptoms (e.g., cough, body aches); empowering to manage your own care. | Can be confusing (which one to pick?); some combinations can have interacting ingredients; doesn’t address severe wheezing. |
| Prescription Medications (e.g., Inhalers) | Directly targets airway inflammation and constriction; much more powerful for wheezing and shortness of breath; prescribed by a doctor for your specific situation. | Requires a doctor’s visit; potential for side effects; may not be necessary for mild cases. |
Let’s break down some specific medications you might encounter:
- Bronchodilators: If you’re experiencing significant wheezing or shortness of breath, a doctor might prescribe an inhaler. The most common one is Albuterol. Think of it as a rescue crew that instantly widens your inflamed airways (the “highways”). It works by relaxing the muscles around the bronchial tubes. The most common side effects are feeling a bit shaky or having a faster heartbeat for a short while after using it.
- Cough Suppressants: For a dry, hacking cough that’s preventing you from sleeping, an OTC suppressant like Dextromethorphan (the “DM” in many cough syrups) can be helpful. It works by telling the cough center in your brain to calm down a bit. A common side effect is drowsiness, so it’s often best for nighttime use. However, if your cough is very productive (lots of mucus), we sometimes want you to keep coughing to clear it out. It’s a balancing act.
- Steroids: In very severe, persistent cases of inflammation, a doctor might prescribe a short course of oral steroids, like Prednisone. This is a powerful anti-inflammatory but comes with more side effects, so it’s reserved for when other treatments aren’t working.
This is a perfect example of how medicine isn’t one-size-fits-all. We tailor the treatment to the person and the severity of their symptoms, just like with other conditions.
Red Flags: When to Call Me (or Any Doctor) Immediately
Most bronchitis is a waiting game. But there are a few situations where you need to stop waiting and seek medical care right away. Please, promise me you’ll pay attention to these:
- High Fever: A fever that goes above 101.5°F (38.6°C) or lasts more than a few days. This could signal a more serious bacterial infection like pneumonia.
- Significant Shortness of Breath: If you’re struggling to breathe, can’t speak in full sentences, or feel like you can’t get enough air, that’s an emergency.
- Sharp, Stabbing Chest Pain: The dull ache of bronchitis is one thing. A sharp pain, especially when you take a deep breath, is a red flag.
- Coughing up Blood: Even a small amount of blood (hemoptysis) needs to be evaluated immediately.
- Symptoms Lasting More Than 3 Weeks: An acute cough should start improving within a couple of weeks. If it’s dragging on or getting worse, it’s time for a re-evaluation.
- Feeling Confused or Disoriented: This can be a sign of low oxygen levels and is a medical emergency.
Frequently Asked Questions My Patients Ask
The virus that caused the bronchitis is contagious, usually for the first few days. The bronchitis itself (the inflammation) isn’t, but you should still cover your cough to avoid spreading the initial virus.
Not necessarily! The color comes from enzymes released by your white blood cells, which are fighting the infection. Green mucus can happen with viral infections, too, so it’s not a reliable sign of a bacterial infection.
When you lie down, mucus can pool in your airways, triggering your cough reflex more easily. Propping yourself up with a few pillows can make a big difference.
This is the frustrating part. The main illness might last a week, but the cough can linger for 2-4 weeks, sometimes even longer, as your airways slowly heal. Be patient with your body.
It’s best to avoid strenuous exercise. Your body needs that energy to heal, and heavy breathing can further irritate your airways. Gentle walking is okay if you feel up to it, but listen to your body.
Unlike acute bronchitis, chronic bronchitis is a long-term condition. However, with lifestyle changes (like quitting smoking) and medical management, symptoms can be controlled very effectively. It is a key component of COPD, which the CDC has excellent resources on.
An expectorant (like guaifenesin) helps thin mucus to make your cough more productive. A suppressant (like dextromethorphan) quiets the cough reflex. Generally, use an expectorant during the day and consider a suppressant at night if the cough is keeping you awake.
My Final Professional Advice
Listen, I know how draining and frustrating this is. You feel sick, you’re not sleeping, and the cough feels like it’s taken over your life. But please hear me when I say this: you will get through it.
Your body is an incredible healing machine. Right now, it’s waging a war in your airways, and it needs your help. Give it the fuel it needs with fluids and good nutrition. Give it the downtime it needs with plenty of rest. Be kind and patient with yourself. This isn’t a race.
Keep an eye out for those red flags we talked about, but don’t let anxiety take over. For the vast majority of people, acute bronchitis is a self-limiting illness that, while deeply unpleasant, runs its course without lasting harm.
You’ve got this. Take it one day at a time. Focus on soothing those airways and letting your immune system do its brilliant work. And please, keep me updated. Don’t hesitate to reach out again if you’re worried or things aren’t improving. That’s what friends—and doctors—are for.
Get some rest.
Warmly,
Dr. Saqlain Mushtaq, MBBS


💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.