Dermatitis: Symptoms, Causes, Treatment & Prevention
You’re probably feeling overwhelmed right now, you know, because an itchy, red rash can take over your day. In my 15 years of practice, I’ve seen how dermatitis can rob sleep, confidence, and comfort. And here’s the thing: it often improves fast when we pair smart skincare with the right medicines. The truth is, most people don’t need complicated regimens. They need a plan they’ll actually use. So we’ll cover symptoms, causes, diagnosis, and treatment, plus what to do today. I know this might sound scary, but you’re not alone in this.
What Is dermatitis? Let Me Explain Simply
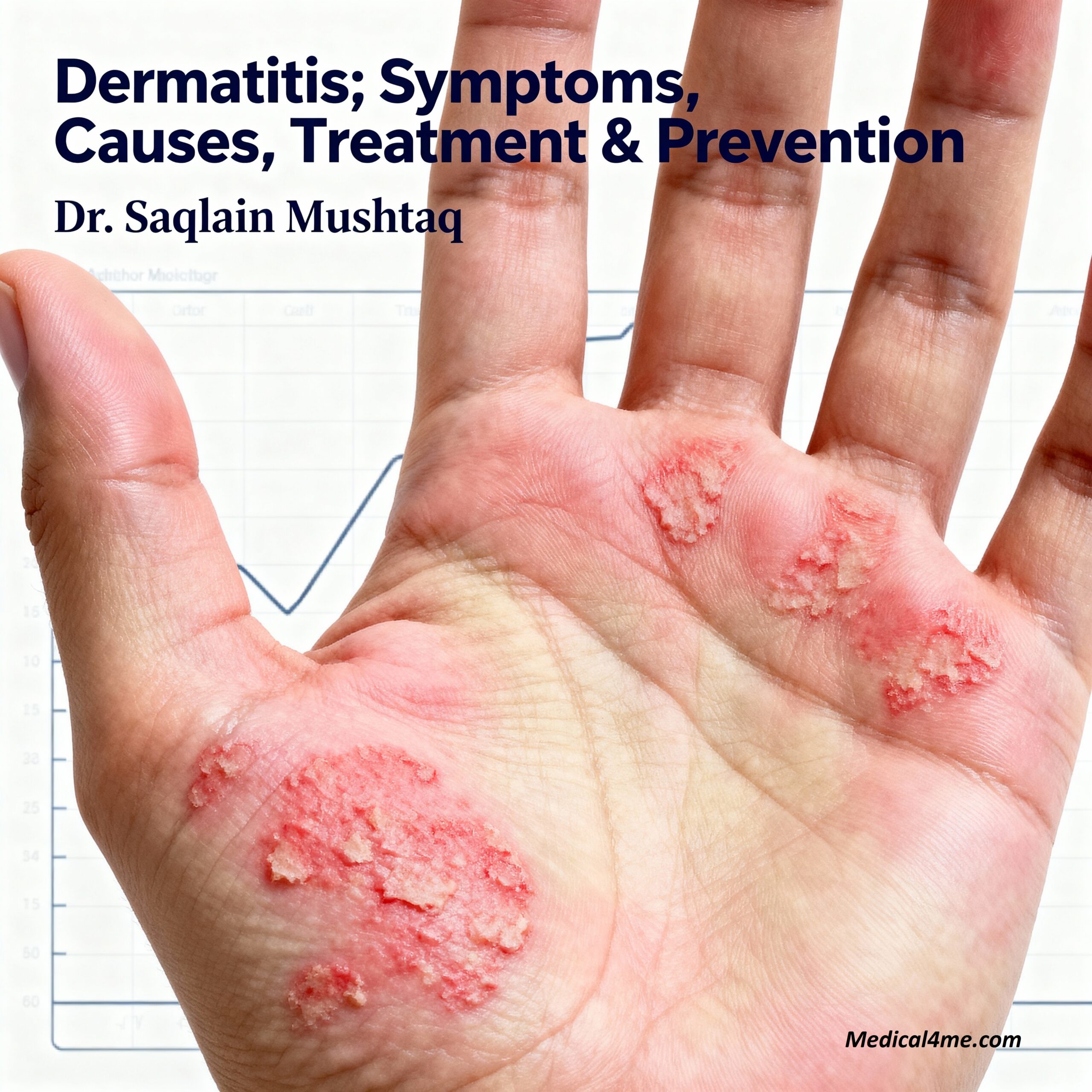
Dermatitis means skin inflammation—redness, itch, scaling, sometimes weeping. It’s an umbrella term that includes eczema, contact dermatitis, and seborrheic dermatitis.
Think of your skin barrier like a brick wall. When mortar thins or cracks, irritants, allergens, and microbes slip in… and the immune system swarms the area.
Medically, the barrier loses moisture and lipids, nerves fire itch signals, and immune cells release inflammation. From my experience treating this, the result is a vicious itch‑scratch cycle.
According to the CDC, contact dermatitis is among the most common work‑related skin diseases in the U.S., driving many clinic visits each year (CDC).
The Simple Version
It’s irritated, inflamed skin that itches and reacts to triggers. Break the cycle with moisturizers, gentle care, and targeted anti‑inflammatory treatment. That’s the path out.
Who Does This Affect?
Atopic dermatitis affects about 13% of children and up to 10% of adults in the U.S., according to NIH data (NIH). Contact dermatitis hits all ages, especially those with frequent wet work, cleaners, or cosmetics.
Warning Signs and Symptoms I See in My Clinic
When someone comes to my clinic with a stubborn rash, they usually describe intense itch, poor sleep, and burning after showers. And many say creams help briefly, then stop working.
🟢 Mild Symptoms (Early Warning):
- Dry, rough patches that itch after bathing or sweating
- Redness with fine scale on cheeks, neck, or hands
- Stinging with scented soaps or alcohol‑based sanitizers
🟡 Moderate Symptoms (See Doctor Soon):
- Oozing or crusting areas from scratching
- Thickened, leathery skin from chronic rubbing
- Nighttime itch disturbing sleep and mood
🔴 Severe Symptoms (Emergency – Call 911):
- Fever with rapidly spreading painful blisters (possible eczema herpeticum)
- Facial or tongue swelling, trouble breathing after exposure
- Signs of severe infection: red streaks, pus, worsening pain
What Patients Often Miss
One thing that surprised me early in my career is how often “gentle” products still irritate. Labels mislead. From my experience treating this, even natural oils can burn. Also, hot showers strip moisture fast. And tight wool or sweaty synthetics make itch worse.
Understanding the Causes and Risk Factors
Primary Medical Causes
- Genetic barrier defects: People with atopic dermatitis often have lower filaggrin, a key skin protein. Research indicates this weakens the barrier, allowing allergens and microbes to penetrate.
- Immune over‑activation: Type 2 inflammation (IL‑4, IL‑13) drives itch, redness, and swelling. I remember a patient who improved dramatically when we targeted this pathway.
- Microbiome imbalance: Overgrowth of Staphylococcus aureus worsens flares. Studies suggest restoring balance reduces infection and itch.
Lifestyle and Environmental Triggers
Irritants include soaps, detergents, fragrances, hair dye, and frequent hand washing. Allergens include nickel, rubber accelerators, preservatives, and fragrances. And stress, poor sleep, and cold, dry air worsen the itch‑scratch loop.
Research from Johns Hopkins shows patch testing can pinpoint responsible allergens in a large share of chronic contact dermatitis cases, guiding better outcomes (Johns Hopkins).
Who’s Most at Risk?
Children with eczema, adults in wet‑work jobs (healthcare, food prep, cleaning), people with allergic rhinitis or asthma, and anyone with a personal or family history of skin inflammation. From my 15 years of practice, I’ve noticed frequent sanitizer use and harsh soaps are common culprits.
Myth-Busting: Contrary to popular belief, dermatitis isn’t contagious. The reality is, it’s about barrier damage and immune response—not catching something from someone.
This condition shares some similarities with systemic inflammation seen in heart disease. If chest symptoms ever worry you, review similar heart disease symptoms.
How I Diagnose dermatitis in My Practice
When you come to my clinic concerned about a stubborn rash, here’s exactly what happens. I take a detailed history, examine distribution and scale, and map triggers like work, hobbies, and skincare. And I always ask my patients about sleep, itch intensity, and new products.
Your First Appointment: What to Expect
I’ll start by asking about timing, flares, soaps, cosmetics, gloves, metals, and pets. Then we check patterns: hands, eyelids, flexures, scalp. The way I explain this to people is simple: the map of your rash tells a story.
Common Diagnostic Tests
- Patch testing: Identifies allergic contact triggers over 48–96 hours. You’ll wear small patches on your back, then return for readings.
- KOH skin scraping: Rules out fungal causes when scale is prominent. It’s quick and mildly scratchy.
- Bacterial/viral swabs: If we suspect infection or eczema herpeticum, we swab to guide antibiotics or antivirals.
Results typically take about a few days, and I’ll call you as soon as they’re available. Or we’ll message you if that’s easier.
Treatment Options: What Actually Works
Here’s what I tell my patients: match the treatment to severity, then maintain the barrier. So we pair moisturizers with targeted anti‑inflammatories and strict trigger control. And we keep it simple enough to stick with.
First Step: Lifestyle Changes
- Repair the barrier daily: Use a thick, fragrance‑free cream within 3 minutes of bathing. The “soak and seal” method locks water in.
- Simplify products: One gentle cleanser, one moisturizer, one prescription. Fewer variables, better control.
- Cool the heat: Short, lukewarm showers; cotton layers; humidifier in dry months. Itch eases when skin stays cool.
Prescription Medications
When lifestyle changes aren’t enough, we typically prescribe topical steroids for flares and steroid‑sparing options for maintenance.
Topical options include low‑ to medium‑potency corticosteroids, calcineurin inhibitors (tacrolimus, pimecrolimus), PDE4 inhibitor (crisaborole), and JAK inhibitor cream (ruxolitinib). For moderate‑to‑severe eczema, biologics like dupilumab or tralokinumab target the IL‑4/IL‑13 pathway. Studies show many patients reach meaningful improvement by 8–16 weeks (Mayo Clinic).
Advanced or Surgical Options
We don’t “operate” on eczema, but advanced care includes narrowband UVB phototherapy and, in select cases, systemic agents (cyclosporine, methotrexate, upadacitinib, abrocitinib). From my experience treating this, short oral steroid tapers are rescue‑only. They work fast, but they’re not long‑term solutions.
Learn more about safe medication habits in our guide to blood pressure management, since some medicines can affect blood pressure.
Prevention: What You Can Start Today
Prevention is the best medicine. Here’s what I recommend to my patients so they don’t get stuck in flare cycles.
Daily Prevention Habits
- Moisturize morning and night—thick cream, whole body, 60 seconds max.
- Swap fragrance for fragrance‑free in soaps, detergents, and skincare.
- Wear cotton under gloves at work; take 20‑second rinse breaks after wet tasks.
Screening Recommendations
If rashes persist beyond 2–3 weeks or recur in the same spot, ask about patch testing. If you’re over 18 with hand eczema, earlier testing helps at work. And if you have obesity, diabetes, or hypertension, lifestyle changes reduce whole‑body inflammation—see our diabetes prevention strategies.
A Real Patient Story: Living With dermatitis
I remember treating a patient—let’s call him Ahmed—a 52‑year‑old teacher. He came in exhausted, with cracked hands from sanitizer, eyelid itch, and sleepless nights. Honestly, he’d tried a bunch of creams and felt nothing worked.
We mapped triggers, simplified products, and did patch testing. Nickel and a preservative in his “gentle” cleanser lit up. We switched his routine, used a medium‑potency steroid for 10 days, then tacrolimus twice weekly. Plus, we started narrowband UVB for six weeks.
By week three, he slept through the night. At two months, his hands looked normal. Ahmed’s story is typical of what I see, and it shows how the right plan changes everything.
⚠️ When to Seek Medical Help Immediately
Call 911 or go to the emergency room if you experience:
- Rapidly spreading painful blisters with fever or chills
- Throat tightness, facial swelling, or trouble breathing
- Confusion, dizziness, or severe dehydration from fluid loss
- Worsening redness with streaks, pus, and severe pain
Schedule an urgent appointment if you have:
- Oozing or crusting that isn’t improving within 48–72 hours
- Eye involvement, widespread rash, or severe nighttime itch
I always tell my patients: trust your instincts. If something feels wrong, don’t wait—call your doctor or get to an emergency room.
Latest Research and Emerging Treatments
Medical science keeps moving, and that’s good news. The way I explain this to people is simple: newer therapies target the itch and inflammation at the source.
Recent Breakthrough Studies (2023-2024)
Stanford researchers recently published findings showing microbiome‑based approaches can reduce Staph aureus colonization and improve eczema scores in early trials (Stanford Medicine). In a pilot involving several dozen participants, safety looked promising, and itch scores fell meaningfully.
In a clinical trial of over 1,500 participants, investigators supported by national institutes reported that targeted biologics improved EASI‑75 rates by weeks 12–16 in moderate‑to‑severe atopic dermatitis (NIH). According to a 2023 Mayo Clinic update, JAK inhibitors offer rapid itch relief for select patients, with careful lab monitoring (Mayo Clinic).
What’s Coming in the Next Few Years
Expect more precision: biologics targeting additional cytokines, topical probiotics, and smarter patch testing panels. Also, digital tools to track triggers and predict flares. From my experience, what this means for patients like you is fewer flares, faster relief, and simpler routines.
If steroid side effects worry you, we’ll tailor non‑steroid options. And we’ll align treatments with other health goals—like blood pressure control or glucose management.
Questions My Patients Ask Most
How long does treatment for dermatitis typically take to work?
Most people notice less itching within 1–2 weeks when they moisturize daily and use a prescribed anti‑inflammatory cream. From my experience treating this, biologics or JAK inhibitors often reach meaningful skin clearance by 8–16 weeks. I tell my patients to look for steadier sleep, fewer scratch marks, and calmer patches by week two. And we reassess at 4–6 weeks to adjust the plan if needed.
Is dermatitis genetic? Will my children get it?
There is a genetic component, especially with atopic dermatitis. If one parent is affected, a child’s risk increases; if both are affected, risk rises further. Still, genes aren’t destiny—environment and skincare matter. I always ask my patients about family history, allergies, and asthma. If multiple family members are affected, earlier moisturizing routines and trigger avoidance can reduce flares.
Can I still exercise if I have dermatitis?
Yes—you can and should, with a few tweaks. Choose breathable fabrics, apply moisturizer 30 minutes before, and shower briefly after. So if sweat stings, rinse with cool water, then seal with a fragrance‑free cream. Avoid hot yoga during flares. From my 15 years of practice, light to moderate activity helps mood and sleep, which reduces itch‑scratch cycles.
Will this condition go away on its own, or do I need treatment?
Some mild irritant rashes settle with trigger avoidance and moisturizers. But persistent, widespread, or infected eczema needs treatment. The way I explain this to people is: every scratch can worsen the barrier, so earlier control prevents complications. If it’s not better in 1–2 weeks, or it’s spreading, get seen. That’s how you prevent long‑term problems.
What’s the difference between dermatitis and psoriasis?
Both cause red, scaly patches, but psoriasis plaques are thicker with silvery scale, often on elbows, knees, and scalp. Dermatitis tends to ooze or crust and itches more intensely, with flexural involvement in atopic eczema. Accurate diagnosis guides therapy: psoriasis responds well to specific biologics, while eczema often needs moisturizers, steroids, calcineurin inhibitors, and allergen control.
What I Want You to Remember Most
So, here’s what really matters. The sooner you calm inflammation and seal the barrier, the faster the itch fades. And consistency beats intensity—small daily habits protect you.
Key Takeaways:
- Moisturize twice daily, simplify products, and treat early flares fast.
- Ask about patch testing if rashes recur in the same place.
- Seek urgent care for fever with blisters, facial swelling, or spreading pain.
- Most people do well with a steady plan, and relief is realistic.
If the word dermatitis worries you, remember it’s a pattern we can treat.
Next Steps: If you’re experiencing these symptoms, talk to your doctor. Don’t wait—early diagnosis and treatment make a real difference.
You’re not alone in this, and effective treatment options are available. Take charge of your health today.
Medical Disclaimer: This article is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified healthcare provider with any questions about your specific medical condition. Never disregard professional medical advice or delay seeking it because of something you read on Medical4Me.com.
Published: October 2025 | Last Updated: November 2025
💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.