Female Sexual Dysfunction — what it is and what you can do
Topic: Female Sexual Dysfunction
If you’re experiencing female sexual dysfunction, you’re not alone. This common condition affects many women and encompasses various challenges with sexual desire, arousal, orgasm, or pain. Understanding the symptoms, causes, and available treatments is the first step toward improving your intimate health.
What is female sexual dysfunction?
Female sexual dysfunction (FSD) is an umbrella term for persistent problems in sexual response, desire, orgasm, or pain that cause distress or relationship difficulty. According to the Mayo Clinic, clinicians break FSD into main categories: low sexual interest/desire, arousal problems, difficulty reaching orgasm, and sexual pain disorders.
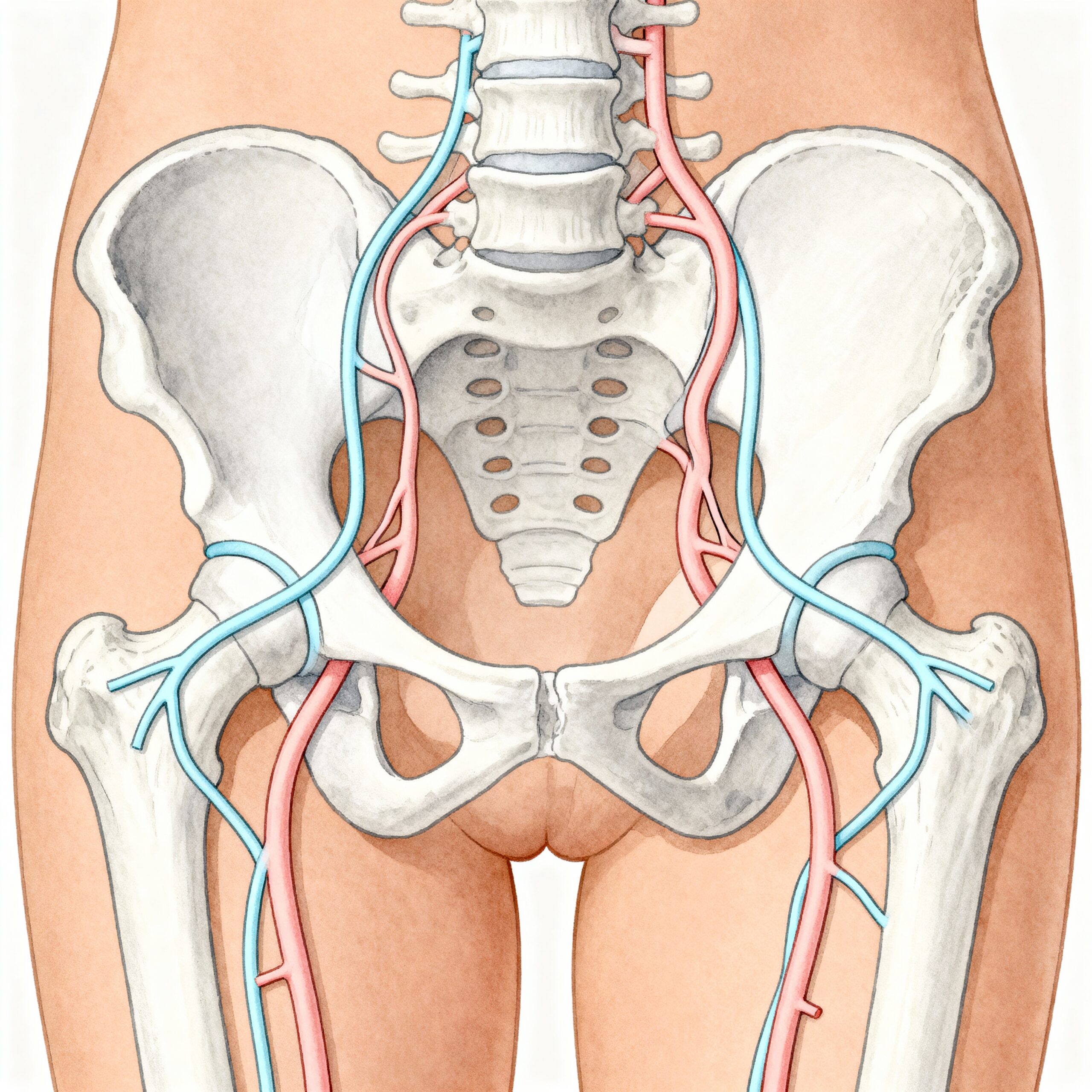
Think of sexual response like a system: hormones, blood flow, nerve signals, mood, relationship context, and certain medicines all play a part. If one or more components are disrupted, sexual experience can change.
Recognizing Symptoms of Female Sexual Dysfunction
Symptoms vary, and severity matters. Use this simple triage to help describe what you’re experiencing:
- 🟢 Mild: occasional low desire or difficulty with arousal that doesn’t cause much distress.
- 🟡 Moderate: ongoing reduction in desire or intermittent pain that affects satisfaction or relationships.
- 🔴 Severe: persistent lack of desire/arousal, inability to orgasm, or pain with most sexual activity that causes major distress.
Tip: When talking with a clinician, describe duration (how long), frequency (how often), relationship factors, health conditions, and medicines — this helps focus evaluation and treatment.
Common specific signs include low or absent sexual fantasies, reduced sexual initiation, decreased pleasure during sex, trouble achieving orgasm, or pelvic pain with intercourse. The Cleveland Clinic outlines these core symptom clusters and their diagnostic thresholds.
Understanding Causes and Risk Factors of Sexual Dysfunction
- Biological: hormonal changes (pregnancy, breastfeeding, menopause), chronic illness (diabetes, cardiovascular disease), neurologic conditions, pelvic surgery, or vaginal/genitourinary atrophy.
- Medication and substance-related: antidepressants (SSRIs), hormonal contraceptives for some people, opioids, alcohol, and recreational drugs can reduce desire or arousal.
- Psychological: depression, anxiety, body image issues, history of sexual trauma can contribute significantly.
- Relationship: communication problems, partner sexual dysfunction, or unresolved conflict often worsen symptoms.
- Socio-cultural: norms, shame, or lack of sexual education affect help-seeking and symptom reporting.
Risk calculator concept: clinicians often weigh age, menopause status, number of chronic conditions, and medication list to estimate likelihood of dysfunction; no single “score” fits everyone.
The Diagnostic Journey for Female Sexual Dysfunction
Diagnosis usually starts in primary care or with a women’s health specialist. Expect a stepwise approach:
- History: sexual history, relationship context, onset, and distress level.
- Medication review: stop or change likely culprits when safe to do so in partnership with the prescriber.
- Physical pelvic exam: look for signs of atrophy, infection, or anatomic causes of pain.
- Targeted tests: labs for thyroid function or sex hormones if indicated; imaging only when specific causes suspected.
- Referral: pelvic pain may need gynecology, vulvar pain specialists, pelvic floor physical therapy, or sexual medicine clinics.
Patient perspective: Many people feel embarrassed to bring this up. A practical opener: “I’ve noticed changes in my sexual desire and it’s worrying me — can we talk about causes and options?” Clinicians recommend routine screening questions in sensitive, non-judgmental language.
Treatment Options for Female Sexual Dysfunction
Treatment is personalized. Below is a comparison of common approaches, their relative effectiveness, and typical side effects or costs.
| Option | Effectiveness (typical) | Notes/costs/side effects |
|---|---|---|
| Psychosexual therapy / CBT | Moderate–High | Addresses mindset/relationship factors; often first-line; cost varies by provider; few side effects. |
| Pelvic floor physical therapy | Moderate | Useful for pain and some arousal issues; requires trained therapist; sessions cost-dependent. |
| Local vaginal estrogen | High for genitourinary symptoms | Preferred for menopausal genitourinary syndrome; low systemic absorption; prescription needed. |
| Systemic hormones (estrogen/testosterone) | Variable | May help some; risks/benefits need specialist discussion; testosterone not FDA-approved for FSD in many countries. |
| Topical lubricants & moisturizers | Helpful (symptom relief) | Low-cost, OTC; first-line for dryness/pain. |
| Devices (e.g., clitoral therapy devices) | Small-moderate | Some show benefit; check reputable product evidence; initial cost. |
| Pharmacotherapy (bremelanotide, flibanserin) | Small-moderate for specific diagnoses | Approved for certain types of hypoactive sexual desire in select populations; side effects and contraindications apply. |
Cost note: Many behavioral therapies are out-of-pocket; some insurers cover pelvic physical therapy or mental health visits depending on plan.
Prevention Strategies for Women’s Sexual Health
- Daily: prioritize sleep, reduce heavy alcohol, check meds annually with prescriber, pelvic floor relaxation exercises.
- Weekly: set a partner “connection” time (phone-free), non-sexual affection, mindfulness practice.
- Monthly: review chronic medication list, schedule primary care or women’s health check if changes noticed.
Lifestyle changes — weight management, smoking cessation, improving cardiovascular health — can meaningfully improve sexual function for many people.
When to Seek Medical Help for Sexual Dysfunction
Red flags (seek prompt care)
- New-onset severe pelvic pain with intercourse
- Any bleeding, drainage, or signs of infection
- Sudden loss of sexual function after surgery or new medication
- Symptoms causing severe distress or relationship harm
If you’re unsure whether symptoms are serious, it’s reasonable to start with your primary care clinician or gynecologist. For urgent pelvic pain or heavy bleeding, seek immediate care.
Patient Story: Overcoming Sexual Dysfunction
Fictional vignette: Sara, 52, noticed painful intercourse and reduced interest after menopause. She tried OTC lubricants but felt embarrassed to tell her doctor. At a routine visit, she described symptoms; her clinician recommended a pelvic exam and low-dose vaginal estrogen. Over three months Sara reported less pain and more comfort during intimacy; she and her partner completed a few sessions of sex therapy to rebuild communication. Outcome: improved function and reduced distress.
This vignette is illustrative only and not a substitute for medical advice. Each person’s situation differs; treatment should be individualized.
Latest Research & Developments in Female Sexual Health

Recent meta-analyses and clinical guidance emphasize that FSD is common across varied populations, that genitourinary syndrome of menopause responds well to local estrogen, and that multidisciplinary care (behavioral + medical) yields the best outcomes for many patients. The American Academy of Family Physicians provides updated guidance on treatment approaches. These studies typically enroll hundreds to thousands of participants and highlight variable prevalence by age and comorbidity.
Frequently Asked Questions About Female Sexual Dysfunction
Many causes: hormonal shifts (pregnancy, menopause), medications (SSRIs), chronic illness, relationship issues, and psychological factors. Often more than one factor is involved. A stepped evaluation helps identify the main contributors.
There are approved medicines for specific diagnoses in select patients (for example, drugs for hypoactive sexual desire disorder under particular approvals). Medications are not a universal fix and work best combined with counseling and lifestyle measures.
Low-dose local vaginal estrogen has minimal systemic absorption and is generally considered safe for genitourinary symptoms when prescribed appropriately; discuss risks with a clinician, especially with a history of hormone-sensitive cancers.
Yes — pelvic floor physical therapy is often effective for pelvic pain and can reduce pain with penetration by teaching relaxation and targeted exercises.
Start with an individual clinician visit or a sexual health counselor. Many therapists offer couple sessions and strategies to open communication safely. You’re not alone — help is available.
💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.