Narcolepsy: Understanding This Complex Sleep Disorder

Roughly two out of every 10,000 people live with narcolepsy, a condition that often hides in plain sight. Many go years—sometimes decades—before getting a clear diagnosis. If you or someone close to you struggles with overwhelming daytime sleepiness, this guide will walk you through what narcolepsy feels like, how it’s diagnosed, and the practical steps that can restore daytime function and safety.
Now, let’s get practical. I write as a clinician who has helped people reclaim their days, and I’ll use plain language, real-world tips, and current treatment options so you can act on what you learn. You’re not alone in this.
What is Narcolepsy?
Medical Definition
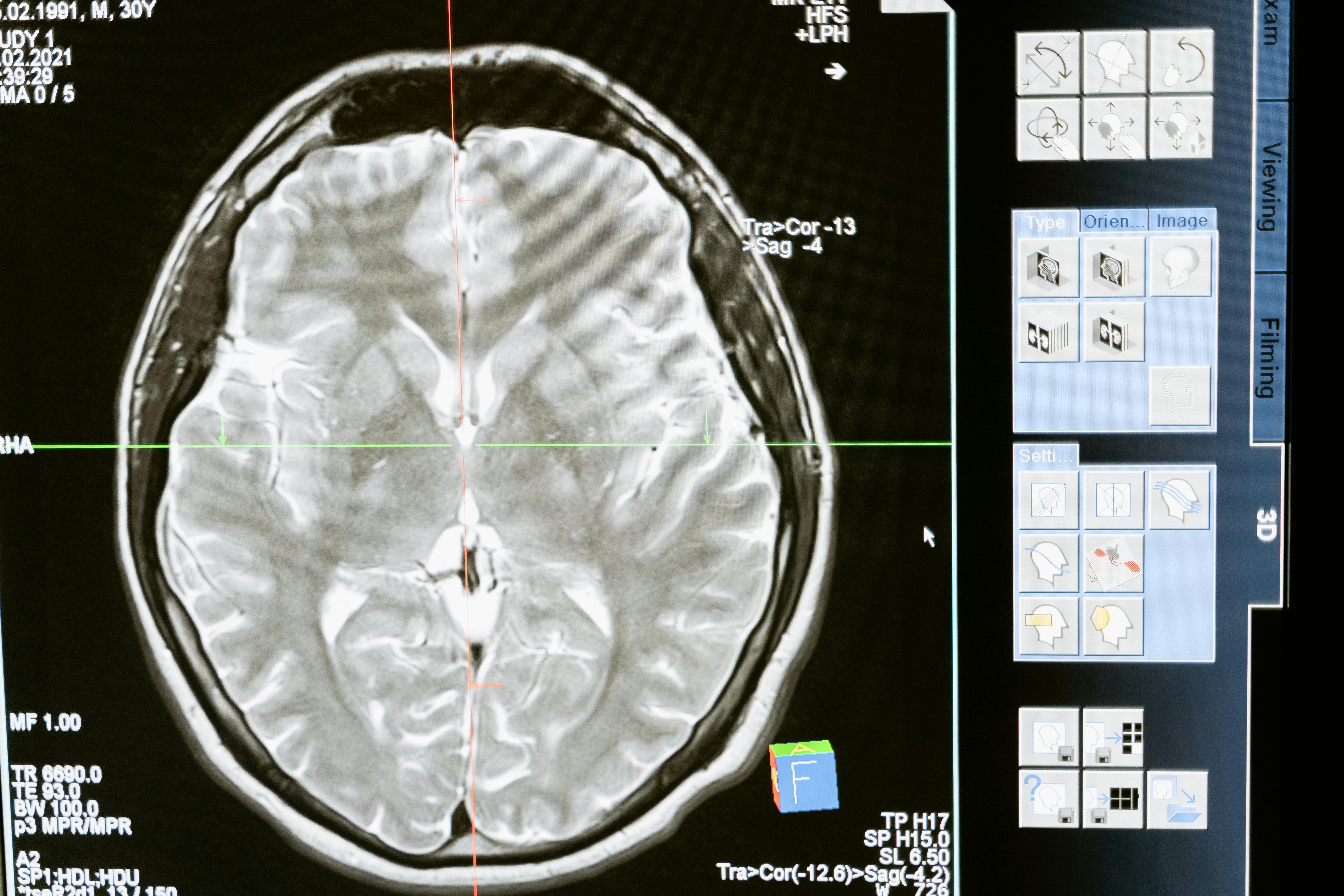
Narcolepsy is a lifelong neurological disorder that disrupts the brain’s control of sleep and wakefulness. It causes severe daytime sleepiness and can let elements of REM sleep appear during waking hours, producing unusual symptoms like cataplexy, vivid hallucinations, and sleep paralysis.
Imagine your brain’s “alert system” is leaky: sometimes it lets you fall asleep when you should be awake, and at other times REM sleep traits—dreams, muscle weakness—spill into wakefulness. That mismatch explains the mix of symptoms people report.
Narcolepsy traditionally divides into two types: type 1 (with cataplexy or very low hypocretin/orexin levels) and type 2 (without cataplexy). Both cause excessive daytime sleepiness, but type 1 often has more dramatic muscle weakness episodes tied to emotion.
Recognizing Symptoms and Signs
Symptoms usually start gradually and can be subtle at first. Many people normalize them for years. Here’s a practical breakdown you can use to spot the disorder early.
Key Symptoms
🟢 Mild: Persistent daytime sleepiness—nodding off in quiet moments, needing longer naps, or feeling mentally foggy despite sleeping at night.
🟡 Moderate: Sleep attacks that occur during activities (talking, eating, meetings). Short naps may temporarily restore alertness, but sleepiness returns quickly.
🔴 Severe: Cataplexy—brief episodes of muscle weakness triggered by strong emotion (laughing, surprise). People remain conscious but may slump, drop items, or briefly collapse.
Other common signs include vivid hypnagogic or hypnopompic hallucinations (dreamlike images or sensations at sleep onset or waking), sleep paralysis (temporary inability to move when falling asleep or waking), and fragmented nighttime sleep. These symptoms are not psychiatric; they are neurologic features of narcolepsy.

Understanding Causes and Risk Factors
The short answer: we don’t yet have a single cause for all cases, but science points strongly to loss of specific neurons and immune triggers.
- Hypocretin/orexin neuron loss: Many people with type 1 narcolepsy have a dramatic loss of the brain cells that produce hypocretin (also called orexin), a chemical that helps maintain wakefulness.
- Autoimmune processes: Evidence suggests an immune attack—likely triggered in susceptible people by infections or other events—targets hypocretin neurons.
- Genetic risk: Certain HLA gene variants raise vulnerability, although most people with those genes do not develop narcolepsy.
- Environmental triggers: Infections, stress, or hormonal changes can be the tipping point for someone already at risk.
- Secondary causes (rare): Brain injury, tumors, or strokes affecting the hypothalamus can produce narcolepsy-like syndromes.
In clinic, onset commonly occurs during the teen years or young adulthood, though symptoms may appear earlier or much later. Recognizing the pattern early improves outcomes.
The Diagnostic Journey
Tip: Start a simple sleep log. Track bedtime, wake time, naps, and any unusual episodes (collapsing, vivid dreams, paralysis). Bring it to your appointment—doctors value concrete examples.
Diagnosis combines careful history with objective sleep testing. Typical steps include:
1. Clinical history—a focused conversation about daytime sleepiness, cataplexy, hallucinations, and sleep paralysis.
2. Overnight polysomnography (PSG)—an in-lab sleep study to rule out other causes like obstructive sleep apnea, which can also cause daytime sleepiness.
3. Multiple Sleep Latency Test (MSLT)—conducted the day after PSG, the MSLT measures how quickly you fall asleep across several scheduled naps and whether REM sleep occurs early. Short average sleep latency and multiple REM onsets support the diagnosis.
4. CSF hypocretin measurement—a lumbar puncture can measure hypocretin levels. Very low levels strongly point to type 1 narcolepsy but this test is used selectively.
5. Blood tests and imaging—sometimes used to exclude other conditions or look for secondary causes.
Diagnosis can be delayed because symptoms overlap with depression, insomnia, medication effects, or lifestyle factors. Persistent, unexplained daytime sleepiness warrants referral to a sleep clinic.
Treatment Options Comparison
| Treatment Type | Effectiveness | Cost Range | Side Effects |
|---|---|---|---|
| Modafinil / Armodafinil | Good for daytime sleepiness (often first-line) | $30–500/month | Headache, nausea, jitteriness in some |
| Sodium oxybate (Xyrem) | Very effective for daytime sleepiness and cataplexy | $5,000–15,000/month (varies by program) | Drowsiness, nausea; requires careful monitoring |
| Methylphenidate / amphetamines | Effective for alertness, older option | $20–200/month | Insomnia, increased heart rate, potential for misuse |
| Pitolisant / Solriamfetol | Newer options with strong efficacy | $500–20,000/year depending on route and coverage | Insomnia, nausea, anxiety; monitor blood pressure |
| Lifestyle and behavioral strategies | Supportive; essential alongside medicine | Low–no cost | None |
Treatment is usually a combination of medicines and behavior changes. Wake-promoting agents (modafinil, armodafinil, solriamfetol) reduce sleep attacks. Sodium oxybate is unique for improving nighttime sleep and markedly reducing cataplexy. Antidepressants are sometimes used to suppress REM-related symptoms like cataplexy. Choice depends on symptoms, comorbidities, cost, and patient preference.
Discuss goals with your clinician: reduce dangerous sleep attacks, control cataplexy, and improve daytime function. Side effects and safety monitoring are important—especially with sodium oxybate and stimulant medications.
Prevention Strategies & Daily Management
You can’t yet prevent narcolepsy, but you can structure your life to limit the impact of symptoms. These practical routines help most people feel more in control.
Daily
- Keep a consistent sleep schedule—go to bed and wake up at the same times each day.
- Plan 1–3 short naps (10–20 minutes) at predictable times when possible.
- Avoid heavy meals and alcohol close to important activities.
- Limit caffeine late in the day; use it strategically if helpful earlier.
Weekly
- Schedule demanding tasks at your most alert hours.
- Plan routes and breaks for long drives; never drive if drowsy.
- Maintain regular physical activity but avoid intense exercise within a few hours of bedtime.
Monthly
- Review symptoms and medication effects with your clinician.
- Adjust work or school accommodations as needed.
- Connect with a support group or counselor for coping strategies.
Small, consistent habits matter more than perfection. A predictable schedule and planned naps often make the biggest difference in daily functioning.
When to Seek Medical Help
Seek Urgent Care If:
- Sudden, severe increases in sleep attacks that cause accidents or injuries
- Long episodes of muscle weakness that don’t remit quickly
- Severe, disturbing hallucinations or safety concerns
- Thoughts of harming yourself or others
- Dangerous medication side effects like breathing problems
Make an appointment with your primary care provider or a sleep specialist if daytime sleepiness limits work, study, or relationships. Early evaluation prevents unnecessary delays and reduces the risk of accidents. If you experience new neurological signs (vision changes, severe headache, seizures), seek immediate medical attention because these might suggest another condition.
Patient Story (Illustrative)
Anna, a 24-year-old graduate student, started nodding off in the library and during class. Her professors thought she was bored, and friends said she needed more coffee. After a year of falling asleep at inconvenient times and experiencing brief episodes where her jaw went slack while laughing, she finally spoke up. Sleep testing confirmed narcolepsy type 1. With a tailored plan—sodium oxybate at night, short daytime naps, and modafinil—Anna regained control of her days and finished her degree. She now mentors others recently diagnosed, reminding them that help is available and recovery of function is possible.
That next-step moment—asking for help—changed her life. You may not need all the same treatments, but having a plan and a specialist makes a big difference.
Latest Research & Developments
Research over recent years has sharpened our understanding and expanded treatment choices. Scientists are investigating immune mechanisms, genetic risk factors, and new therapeutics aimed at restoring or mimicking hypocretin function.
Clinical trials of once-nightly sodium oxybate formulations and newer wake-promoting drugs have expanded options for patients. Early-stage work on hypocretin replacement or immune-targeted therapies holds promise but remains experimental.
Awareness and diagnostic tools continue to improve; many regions report rising rates of diagnosis as clinicians recognize the condition more readily.

Frequently Asked Questions
Living Well with Narcolepsy
Living with narcolepsy means learning how to work with your body. That can include negotiating workplace accommodations, creating sleep-friendly routines, and building a support system. Many people with narcolepsy hold demanding jobs, raise families, and enjoy rich social lives.
Know your rights—workplace protections exist, and reasonable accommodations like flexible hours or scheduled breaks can make a major difference. Peer support groups and online communities also offer practical tips and emotional support.
Finally, be patient in finding the right medication mix. Treatment is rarely one-size-fits-all; a gradual, collaborative approach with your clinician typically yields the best results.
Conclusion
Narcolepsy is a challenging but manageable condition. Recognizing symptoms early, pursuing appropriate testing, and building a realistic treatment plan improve safety and quality of life. If daytime sleepiness or sudden muscle weakness affects your life, start by keeping a simple sleep diary and asking for a referral to a sleep specialist.
You don’t have to accept constant fatigue. With the right team and tools, most people with narcolepsy regain control of their days and pursue their goals.
Take the first step: track your symptoms, reach out for medical help, and connect with others who understand the journey.
Medical Disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on Medical4Me.com.

💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.