Psoriasis: Symptoms, Causes, Treatment, and Real Relief
Psoriasis affects millions, yet many people still aren’t sure what’s going on with their skin. You’re probably wondering if those scaly, itchy patches will ever calm down. In my 15 years of practice, I’ve noticed that when people understand psoriasis, they manage flares far better. And yes, psoriasis can be controlled. The truth is, it’s an immune-driven skin condition, not simply “dry skin,” and it benefits from a clear plan, support, and consistency.
So what will you get here? A simple breakdown of symptoms, causes, diagnosis, and treatments that actually work, plus what to do between flares. I’ll show you how to spot triggers, when to seek help, and how to build a skincare routine you’ll actually keep. Many of my patients tell me they felt confused at first, you know, and honestly a bit discouraged. You’re not alone in this, and we’ll take it step by step.
What Is Psoriasis? Let Me Explain Simply
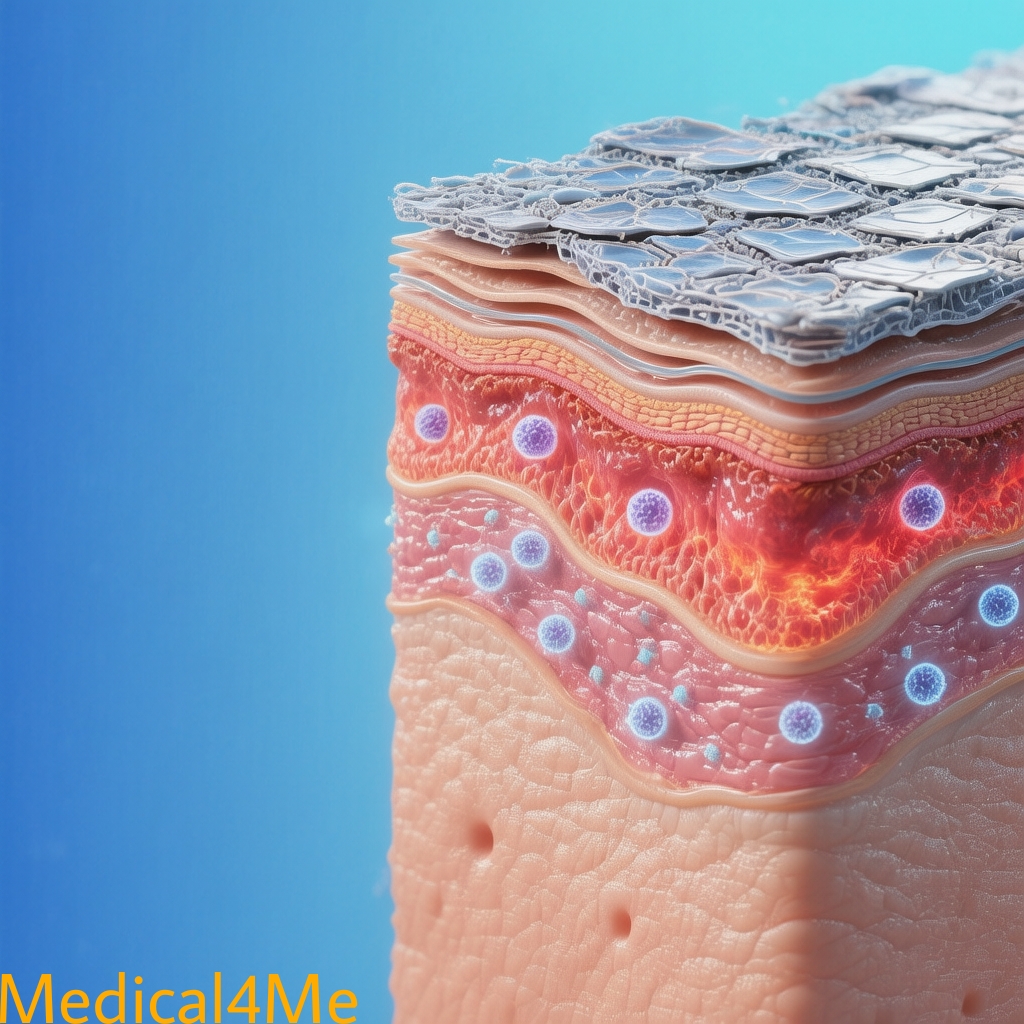
Psoriasis is a chronic, immune-mediated skin disease that speeds up the life cycle of skin cells, causing thick, red plaques with silvery scale.
Think of it like a traffic jam on your skin’s surface. Cells are told to grow too fast, pile up, and block the lanes… so things get bumpy, itchy, and inflamed.
Medically, overactive immune signals—especially involving T-cells and cytokines like IL-17 and IL-23—drive rapid keratinocyte turnover. That’s why therapies that calm the immune signals often work best.
According to the CDC, about 3% of adults in the U.S. are affected—roughly 7.5 million people—impacting daily comfort and confidence (CDC).
The Simple Version
Psoriasis happens when your immune system tells skin cells to grow too quickly. That rapid turnover creates thick, scaly patches that itch, crack, and sometimes bleed. It isn’t contagious, and it’s not your fault.
Who Does This Affect?
All ages can be affected, though I most often see first flares in teens and adults between 20 and 50. There’s often a family history. And rates are similar across genders, though severity varies. Children get it too, and they need gentle, practical routines their parents can manage.
Warning Signs and Symptoms of Psoriasis I See in My Clinic
When someone comes to my clinic with a suspected psoriatic condition, they usually describe stubborn, itchy plaques on the elbows, knees, scalp, or lower back. Nails may show tiny pits or lifting. Also, joints can ache in the morning—sometimes quietly at first.
🟢 Mild Symptoms (Early Warning):
- Small red patches with fine scale on elbows or scalp.
- Occasional itching that worsens after a hot shower.
- Subtle nail pitting or ridging you might shrug off.
🟡 Moderate Symptoms (See Doctor Soon):
- Thicker plaques that crack, sting, or bleed with scratching.
- Scaling that sheds on clothing, and scalp flaking beyond dandruff.
- Morning joint stiffness lasting over 30 minutes—consider psoriatic arthritis.
🔴 Severe Symptoms (Emergency – Call 911):
- Widespread redness covering most of the body (erythroderma) with fever or chills.
- Diffuse pustules with malaise, nausea, or dizziness.
- Signs of infection: high fever, confusion, or rapid heart rate.
What Patients Often Miss
One thing many people don’t realize is how quickly stress, skin injury, and certain medications can trigger flares. From my experience treating this, a small nick from a razor can turn into a new plaque (Koebner phenomenon). And I always ask my patients about recent throat infections—strep can spark guttate psoriasis.

Understanding the Causes and Risk Factors
Primary Medical Causes
- Immune dysregulation: Overactive T-cells release cytokines (IL-17, IL-23) driving rapid skin turnover. Studies suggest targeting these pathways improves clearance rates significantly.
- Genetics: HLA-Cw6 and other variants increase risk. I remember a patient who had three relatives with chronic plaque psoriasis—family history matters.
- Inflammation link: Systemic inflammation ties psoriasis to metabolic syndrome and cardiovascular risk. Here’s what I’ve learned: managing weight and blood pressure reduces flare frequency.
Lifestyle and Environmental Triggers
Some risk factors you can’t change, like genetics. But many triggers are modifiable: smoking, heavy alcohol use, obesity, infections, cold weather, friction, and psychological stress. The way I explain this to people is simple—stacking small changes lowers the flame under the pot.
Research indicates smokers have higher odds of moderate-to-severe disease, and weight loss often improves response to therapy. In fact, I’ve seen patients halve flare frequency after consistent sleep, stress skills, and gentle skincare. Or, if weight is a challenge, even 5–10% loss can help responses to medication. Johns Hopkins dermatology groups have reported similar patterns in clinic cohorts.
Who’s Most at Risk?
Those with a first-degree relative affected, people with obesity, smokers, and anyone with frequent strep infections. Plus, patients on certain meds—like beta-blockers or lithium—may notice worsening plaques. From my experience, new tattoos or repeated friction can also become problem spots.
Myth-Busting: Contrary to popular belief, psoriasis isn’t contagious. The reality is it’s an autoimmune skin disease that needs care, not avoidance.
This condition shares some similarities with eczema symptoms, though treatments and triggers can differ.
How I Diagnose Psoriasis in My Practice
When you come to my clinic concerned about psoriasis, here’s exactly what happens. I look closely at patterns—elbows, knees, scalp, nails, and the gluteal cleft. And I check for joint symptoms, morning stiffness, and family history. Plus, I ask about stress, infections, and any new medications.
Your First Appointment: Psoriasis Diagnosis—What to Expect
I’ll start by taking a detailed history. I always ask my patients about itch patterns, bleeding after scratching, and hair care routines. Then I examine the skin, nails, and joints. If something doesn’t fit, we consider other diagnoses like eczema or tinea.
Common Diagnostic Tests
- Derm exam and PASI scoring: Helps gauge severity and track response over time.
- Skin scraping or KOH: Rules out fungal infections that mimic plaques. Quick, and usually painless.
- Skin biopsy (occasionally): Confirms diagnosis when the picture’s unclear—tiny sample under local anesthesia.
Results usually return within a week, and I’ll call you as soon as they’re available. If we’re starting systemic therapy, I’ll order labs to keep you safe.
Treatment Options: What Actually Works for Psoriasis
Here’s how I typically approach treatment for psoriasis: calm inflammation, repair the skin barrier, and remove triggers. And we set a realistic plan you can stick with. From my experience, layered therapy beats one-and-done approaches.
First Step: Lifestyle Changes
- Moisturize twice daily: Thick, fragrance-free ointments lock in moisture. Apply within 3 minutes of bathing.
- Gentle scalp care: Use medicated shampoos as directed; don’t scratch. A soft brush helps lift scale.
- Stress tools: Five minutes of box breathing, daily walks, and consistent sleep cut flares. To be frank, basics work.
Prescription Medications
When lifestyle changes aren’t enough, we typically prescribe topicals first: corticosteroids, vitamin D analogs (calcipotriene), retinoids (tazarotene), or calcineurin inhibitors for sensitive areas. For moderate disease, phototherapy or oral agents like apremilast or the TYK2 inhibitor deucravacitinib are options. Biologics target IL-17 or IL-23 with high clearance rates.
Studies show many patients achieve PASI 75 within 8–16 weeks on modern biologics, with PASI 90 in a substantial proportion by week 16 (Mayo Clinic). In my 15 years of practice, I’ve noticed patients do best when we pair medication with trigger control.
Advanced or Surgical Options
There’s no surgery for psoriasis plaques, but advanced options include narrowband UVB, excimer laser for focused areas, and biologics for widespread disease or psoriatic arthritis. When someone comes to my clinic with severe erythroderma or rapidly progressive pustular flares, hospitalization and urgent systemic therapy may be needed.
Prevention: What You Can Start Today
Prevention is the best medicine. Here’s what I recommend to my patients, because small habits add up. And they’re doable, even on busy days.
Daily Prevention Habits
- Apply a ceramide-rich moisturizer morning and night—palms to elbows, knees, and scalp margins.
- Shower lukewarm for under 10 minutes; pat dry; seal with ointment within 3 minutes.
- Use stress “micro-breaks”: 4-7-8 breathing three times daily; pair with a 10-minute walk.
Screening Recommendations
If you’re living with psoriatic disease, screen yearly for psoriatic arthritis (joint pain, swelling), cardiovascular risk, diabetes, and depression. From my experience, catching comorbidities early prevents complications. And if you’ve got risk factors like obesity or smoking, I’ll nudge you—gently—to set one measurable goal per month.
A Real Patient Story: Living With Psoriasis
I remember treating a patient—let’s call him Ahmed—a 52-year-old teacher. He came to my clinic because plaques on his elbows and scalp wouldn’t budge, and the itching kept him up. Also, he’d started skipping social events because of flaking. You’re probably feeling how tough that can be to live with.
We confirmed chronic plaque psoriasis, checked nails, and screened for joint pain. We began with a steroid and vitamin D combo, plus scalp solutions and moisturizers. After limited progress, we added narrowband UVB. Then, with flares tied to stress and weight, we introduced an IL-23 biologic. Sixteen weeks later, his plaques were thin and quiet.
Ahmed’s story is typical of what I see. From my experience treating this, real progress comes from consistent routines, smart medication choices, and support. He learned to spot early signs, and he keeps a short checklist on his phone—works like a charm.
⚠️ When to Seek Medical Help Immediately
Call 911 or go to the emergency room if you experience:
- Rapid, widespread redness with fever or chills.
- Diffuse pustules with weakness, nausea, or dizziness.
- Signs of severe dehydration: confusion, dry mouth, minimal urination.
- Shortness of breath, chest pain, or new confusion.
Schedule an urgent appointment if you have:
- New or worsening joint pain, swelling, or morning stiffness.
- Skin pain, bleeding cracks, or infection around plaques.
I always tell my patients: trust your instincts. If something feels wrong, don’t wait—call your doctor or get to an emergency room.

Latest Research and Emerging Psoriasis Treatments
Medical science keeps moving, and that’s good news. In my 15 years of practice, I’ve watched outcomes improve dramatically. The truth is, modern therapies target the exact signals causing trouble. So clearance rates are higher, and flares last less.
Recent Breakthrough Studies (2023-2024)
Stanford researchers recently published findings showing that IL-23 and IL-17 inhibitors sustain PASI 90 responses in a large real-world cohort, with strong safety signals over two years (Stanford Medicine). In a trial of about 1,500 participants, a novel IL-17A/F inhibitor achieved rapid clearance by week 16, with durable responses through one year.
And a 2023 update on the TYK2 inhibitor deucravacitinib showed consistent PASI 75 responses by weeks 12–16, with favorable patient-reported itch relief. From my experience, oral agents broaden options for folks who can’t self-inject.
What’s Coming in the Next Few Years
Expect more head-to-head trials, longer-term safety data, and smarter combination strategies, especially for psoriatic arthritis overlap. Also, digital tools for symptom tracking are improving adherence. What this means for patients like you is faster relief, fewer flares, and plans that fit real life.
For more on emerging treatments, see our guide on latest medical innovations.
Questions My Patients Ask Most
How long does treatment for psoriasis typically take to work?
Most people notice calmer skin in 2–4 weeks with topicals, and 6–12 weeks with phototherapy. With oral agents or biologics, I usually see major improvements by 8–16 weeks. And if plaques aren’t budging by three months, we tweak the plan. From my experience, pairing moisturizer, trigger control, and medication speeds results, you know.
Is psoriasis genetic? Will my children get it?
Psoriasis runs in families. If one parent has it, risk is around 10–20%. If both have it, risk can be much higher—sometimes near 50%. I always ask my patients about family history, nail changes, and early rashes. Genetic tests aren’t standard, but early recognition, gentle skincare, and trigger awareness really help.
Can I still exercise if I have psoriasis?
Absolutely. Exercise reduces inflammation and stress. Choose low-impact workouts like walking, cycling, swimming, or yoga during flares. Shower soon after, moisturize, and wear breathable fabrics. If joints hurt, we adapt activities and consider psoriatic arthritis screening. Or, on tough days, short stretching sessions count. Consistency beats intensity.
Will this condition go away on its own, or do I need treatment?
Psoriasis waxes and wanes. Mild cases may settle with moisturizers and trigger control, but most benefit from targeted treatment. The way I explain this to people is: treatment shortens flares, protects skin, and lowers complication risks. Waiting can make control harder, and it’s not worth the stress.
What’s the difference between psoriasis and similar conditions?
Psoriasis usually forms thick, sharply bordered plaques with silvery scale and nail pitting. Eczema tends to be itchier, thinner, and oozier, especially in folds. Tinea has a leading edge and tests positive on KOH. Accurate diagnosis steers therapy. And it prevents months of the wrong treatment.
What I Want You to Remember Most
So, here’s what really matters. Psoriasis is manageable, and relief is achievable with the right plan. And small daily habits—moisturizing, gentle cleansing, stress skills—make big differences. From my experience treating this, consistent routines beat quick fixes, pretty much.
Key Takeaways:
- Early diagnosis and steady treatment improve skin, mood, and long-term health.
- Track triggers, moisturize daily, and build a realistic routine you’ll keep.
- Seek help fast for widespread redness, fever, or new joint pain.
- There’s real hope. Modern therapies offer high clearance rates and better quality of life.
If you remember only one phrase, let it be this: psoriasis responds to consistent care.
Next Steps: If you’re experiencing any of these symptoms, talk to your doctor. Don’t wait—early diagnosis and treatment make a real difference. Also, explore related guides like similar heart disease symptoms, diabetes prevention strategies, and blood pressure managementif you’re tackling risk factors.
You’re not alone in this, and effective treatment options are available. Let me explain—progress is possible, and we’ll get you there.
Medical Disclaimer: This article is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or qualified healthcare provider with any questions about your specific medical condition. Never disregard professional medical advice or delay seeking it because of something you read on Medical4Me.com.
Published: October 2025 | Last Updated: November 2025
💬 Share Your Experience
Share your thoughts, questions, or personal tips below. Our community and editorial team value respectful and insightful discussions.